Pancreas
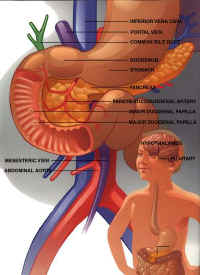 The pancreas is a gland that is located behind the stomach. As part of the digestive system, the pancreas produces juices with enzymes that help the body digest food (an exocrine function). The pancreas also produces a hormone called insulin (an endocrine function). Insulin helps control the amount of sugar, or glucose, in the blood.
The pancreas is a gland that is located behind the stomach. As part of the digestive system, the pancreas produces juices with enzymes that help the body digest food (an exocrine function). The pancreas also produces a hormone called insulin (an endocrine function). Insulin helps control the amount of sugar, or glucose, in the blood.
To supply energy that the body needs, the digestive system changes some foods into a simple sugar called glucose. Glucose is absorbed into the blood stream and circulated to the cells of the body.
For glucose to be used by the body cells, insulin must be present. Insulin acts like a key that unlocks the cells and allows glucose to enter.
When things go wrong
The most common problem related to the endocrine function of the pancreas is diabetes mellitus. Diabetes is a condition in which either the pancreas does not produce enough insulin, or the cells of the body are unable to use the insulin. Without insulin, the body cannot use glucose for energy. Blood glucose levels become very high, a condition called hyperglycemia. Symptoms of diabetes include constant thirst, frequent urination, increased appetite, weight loss and poor growth, blurred vision, frequent infections, and slow healing.
In type I diabetes, the body fails to make enough insulin. Type I diabetes, the type that usually affects children, is called insulin-dependent diabetes because daily insulin injections are needed to control it.
Type II diabetes is more common and develops gradually, usually in people who are over age 40 and overweight. In many cases, the pancreas is producing enough insulin, but for some reason the cells cannot use it. This form of diabetes may be controlled by a careful diet, exercise, and maintaining a normal body weight. Oral medications or insulin injections may also be needed.
Managing type I diabetes
The goal of treatment is to keep blood glucose levels near normal. This is done by injecting synthetic insulin into the blood stream. There should be a careful balance of insulin, foods eaten, and physical activity. Maintaining this balance can be difficult, and it is likely that there will be times when blood glucose levels get too low, a condition called hypoglycemia.
Symptoms usually come on suddenly and may include nervousness and shaking, sweating, dizziness, weakness, and hunger. This must be treated promptly or loss of consciousness may occur. To treat, give the child glucose tablets or something to eat or drink with a high sugar content such as regular soda, juice, honey, or hard candies.
and families must learn how to give insulin injections and test glucose levels daily. This is very important, as insulin needs may change during times of illness, stress, unusual activity, or growth spurts.
It is usually best to get help from health care professionals who specialize in treating diabetes. They can provide medical care, information, practical advice, and help with emotional and social concerns.
Special considerations
After many years, diabetes can damage the eyes, kidneys, nerves, and blood vessels. The risk of developing these complications can be lowered a great deal by keeping blood glucose levels in the normal range.
- The pancreas is a gland that is part of the digestive system
- Exocrine function
- Islets of Langerhans in the pancreas produce two hormones
- Endocrine function
- Insulin – stimulates cells to take up glucose from the blood; promotes the storage of glucose, fatty acids, and amino acids; lowers blood glucose levels
- Glucagon – activity is opposite that of insulin: glucagon promotes the release of glucose, fatty acids, and amino acids from storage into the bloodstream; raises blood glucose levels
- Insulin and glucagon work together to keep blood glucose level normal
- Normal insulin levels are essential for normal growth
Disorders and clinical features
- Type I diabetes or insulin-dependent diabetes mellitus (IDDM)
- Excessive thirst, excessive urination
- Rapid weight loss, poor growth
- Hyperglycemia and ketosis (usually Type I)
- Fasting blood glucose >140 mg/dL
- Infection prone
- Slow healing
- Type II or non-insulin-dependent diabetes mellitus (NIDDM)
Therapy
- Diet, exercise, insulin for Type I
- Diet, exercise, oral hypoglycemics and/or insulin for Type II
Managing diabetes
- Self-monitoring of blood glucose
- Balance of diet, exercise, and insulin
- Injection technique
- Long-term complications awareness
- Cardiovascular
- Renal
- Ophthalmologic
- Peripheral
- Glycohemoglobin monitoring
- Psychosocial factors at developmental stages
- Emotions
- Body awareness/image
- Physical exercise and activity
