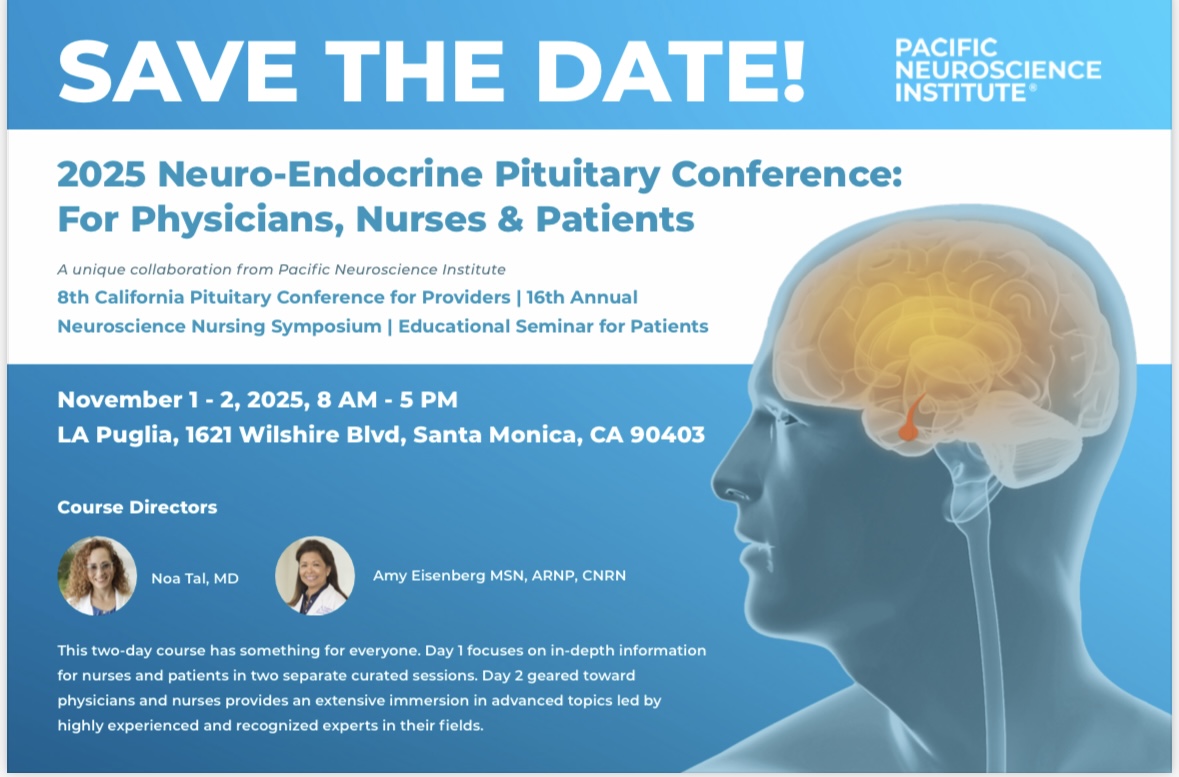
Don’t Miss Our Exciting Upcoming Events!
Nominate for Gentle Giant Award!
Do you have a pituitary HCP who has made a profound difference in your care or your life? A real “Gentle Giant”. We want to hear about them! Help us recognize the amazing professionals who go above and beyond by nominating your favorite doctor. Your story can help shine a light on the heroes in our community and inspire others on their journey. Submit your nomination today—we can’t wait to celebrate them with you!
Discover Leading Professionals and Specialized Services in Healthcare
Search
Recent Webinar
Patient’s Corner
Introducing Patient’s Corner, a place for you, the patient, to share your stories. If you have a story you would like to share please contact us below.
PNA Spotlight: Dr. Jamie Van Gompel
This month the PNA Spotlight focuses on longtime PNA member Dr. Jamie Van Gompel, a neurosurgeon at Mayo Clinic in Rochester, Minnesota. Dr. Van Gompel earned a B.S. in molecular biology, biochemistry, medical microbiology and immunology, and then his M.D. at the University of Wisconsin. He earned a certificate in Clinical and Translational Research at Mayo Clinic, where he also did residencies as a clinician investigator and in neurologic surgery. He then completed a fellowship in skull base and complex cranial surgery at the University of South Florida. He was kind enough to answer some questions from the PNA.
Tell us about your educational journey.
At the University of Wisconsin as an undergraduate, I did a couple of majors, including molecular biology, immunology and medical microbiology and then biochemistry. When I found out at college that you could pay the same amount and take over 18 credits, I would load up, so I got all those in four years. In between my undergraduate work and medical school, I worked for the National Institutes of Health (NIH) for a period of time. I was really interested in infectious diseases, so I worked at the Rocky Mountain Lab in Montana, researching bacteria. It served as a high-level pathogen facility, much like the one at the Centers for Disease Control in Atlanta. So, it’s a cool place to work; I really enjoyed it. And then we could go fly fishing at lunchtime on the river. It was fun.
Later, I went to University of Wisconsin at Madison for medical school. I started out wanting to be a general surgeon, and I was very interested in neuroendocrine diseases. I was working on carcinoid tumors and medullary thyroid tumors, because I thought that it was really cool to tackle a challenging surgical disease, with secreting tumors; something that has medical impact. I even took a year doing a Howard Hughes Fellowship in research with my mentor Dr. Herb Chen, which was very formative after my clinical year in medical school (year 3). It was during this formative time that I decided to transition my interest from general surgery to neurologic surgery.
I finished medical school and came up to Mayo Clinic in Rochester, Minnesota for my residency. I did a seven-year residency here, and as part of my education within that, I did the Translational Studies Program, which teaches people how to do research and clinical trials. I was asked to stay on staff here as a skull-base and epilepsy neurosurgeon. I did a complex cranial fellowship with Dr. Harry van Loveren in South Florida.
At the end of that fellowship, I was playing softball with USF in New York City, and I broke my hand. This led to more education, since I broke my hand before I started at Mayo Clinic. My boss, mentor and chair at Mayo Clinic at the time, Dr. Fred Meyer, said, “Hey, since you broke your hand, you can’t operate. I’ll send you around. What do you want to do?” And I said, “Well, I’d like to go see all these big-time people in pituitary surgery from across the world.” So, I traveled to see Paulo Cappabianca and Luigi Cavallo out in Napoli, Italy. I was also able to visit with people like the Pittsburgh group (Paul and Juan), Dan Prevedello at OHSU and Ted Schwartz in New York. I was able to sample how everyone was doing pituitary surgery at the time. My hand healed and I returned to Mayo Clinic; that was 14 years ago. It kind of backs the Taoist fable of the Chinese man who lost his horse, in which when something bad happens but it turns out alright. When I broke my hand, it seemed bad, but in this circumstance, it turned out to be a blessing. So, you just never know how things will work out.
Who were your primary mentors?
I think all of us have a ton of mentors. I’ve always admired Dr. Ed Laws. I’ve always looked up to his work, because he started at Mayo Clinic and was very interested in pituitary disease, as I am. Also, Drs. Fred Meyer and John Atkinson, two pituitary surgeons at Mayo Clinic, are big mentors of mine here who taught me a lot. And my other mentors are Dr. Van Loveren, Dr. Agazzi, and Dr. Sammy Youssef, who were in South Florida. I want to acknowledge Dr. Michael Link, who’s here at Mayo Clinic as well.
Why choose pituitary surgery?
I love doing pituitary surgery. I tell a lot of my patients that if I if I got independently wealthy tomorrow, if I hit the Powerball, I would still be a neurosurgeon and perform pituitary tumor surgeries. I might even pay people to be able to do the surgery! I really enjoy the complexity of it, not only the surgical complexity, but also the management of the patients, pre- and post-operatively. I like the fact that we can help them improve for the rest of their lives.
What do you see as the future of your field?
We are trying to understand what gives us good outcomes, and how we can improve that. I think there’s a lot of progress to be made with machine learning and Artificial Intelligence (AI), which we can use to help patients diagnosed with pituitary tumors. Right now, we do a lot of data granularity, through Mayo Clinic and a database that we developed called MAPER, the Mayo Adenoma Pituitary Enterprise Registry. We also work with the RAPID Consortium. These are trying to collect large amounts of data to determine what really, truly impacts pituitary outcomes for patients. Also, I’m fortunate enough at Mayo Clinic to see also the very uncommon cases, and we still study them quite a bit to see how we can do better with those as well. The focus of my research is just better patient outcomes, and that includes not only having the tumor gone, but better endocrine outcomes and better life outcomes for patients.
Is there a role for robotics in pituitary surgery?
We use robots, but not for pituitary surgery. Nowadays, we’re using it for epilepsy and some other things. I don’t think that pituitary surgery is going to be supplanted by some super robot in the future, very soon. But I do think that AI is integrating data and seeing things at a pace that people just can’t. I think that AI is going to be an important thing for all medical fields. And pituitary medicine will benefit from that. I think good pituitary surgeons can look at things and do a lot of risk assessments. Most of these things will be just aiding pituitary surgeons in their risk assessment and can put all the data at their fingertips. It will help enhance our memory to understand how good our outcomes can be, or maybe to be more realistic in some circumstances.
We have seen great progress in pituitary medicine. Maybe 10 years ago we would have removed a little bit of the tumor and left some behind. Whereas nowadays we can, at the same risk, remove all the tumor and avoid other therapies that they just couldn’t do back then. We can credit technological advances and a better understanding of the anatomy and of medical treatments.
Why are you involved with the PNA?
I love the PNA’s mission. Doctors sometimes talk at such a high-level, and we need to really connect with patients. The PNA helps us prioritize what’s important to the patients and hear what they’re saying and what they need. The information is modeled in a different way that isn’t so technical. I think it is really important to have patient-facing enterprises like PNA. I’ve been a PNA member now for over 13 years, and I think that I’ve learned as much from the PNA as they’ve learned from me.

“I love doing pituitary surgery. I tell a lot of my patients that if I if I got independently wealthy tomorrow, if I hit the Powerball, I would still be a neurosurgeon and perform pituitary tumor surgeries.”
Get Involved
If you wish to donate, contact:
- P.O. Box 1958, Thousand Oaks, CA 91358
- Office: 805.499.9973
- Fax: 805.480.0633
- Email: [email protected]
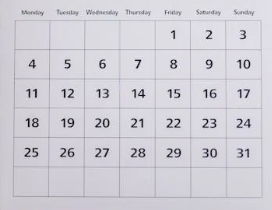
Coming Events

Volunteer With Us

Pituitary Patient Toolkit

Seventh Edition - Now Available!
The Pituitary Patient Resource Guide Seventh Edition is now available! Be one of the first to have the most up-to-date information.
The Pituitary Patient Resource Guide a one of a kind publication intended as an invaluable source of information not only for patients but also their families, physicians, and all health care providers.
It contains information on symptoms, proper testing, how to get a diagnosis, and the treatment options that are available. It also includes Pituitary Network Association’s patient resource listings for expert medical care.
Latest News
May 2023 Research Articles
Pituitary TumorsPituitary adenoma consistency affects postoperative hormone function: a retrospective study.Diagnosis and Management of Pituitary Adenomas: A Review.High-Grade Ectopic Pituitary...
News Articles May 2023
WWE Wrestler Discusses his Pituitary Journey WWE Wrestler Tolulope "Jordan" Omogbehin, known as Omos or the Nigerian Giant, discusses his diagnoses of acromegaly and a form of Cushings, along with...
PNA Medical Corner: Fascia Lata in Reconstructive Neurosurgery
This month the PNA Medical Corner showcases an article co-authored by a member of the PNA, Dr. Varun Kshettry of the Cleveland Clinic. The study concludes that the use of fascia lata in challenging...