News Articles February 2022
Written on 04 February 2022.
August 2022 Research Articles
Pituitary Surgery
Free Tissue Transfer for Skull Base Osteoradionecrosis: A Novel Approach in the Endoscopic Era
Editor’s note: Dr. Kshettry is a member of the PNA.
Minimally invasive keyhole techniques for resection of giant intracranial tumors.
Pituitary and COVID-19
Encephalitis due to COVID-19 in a Patient Who Has Undergone Transsphenoidal Pituitary Surgery.
Pituitary Apoplexy
Revisiting Pituitary Apoplexy.
Pituitary Tumors/Morphology
Hormonal Health
Pituitary hormone α-MSH promotes tumor-induced myelopoiesis and immunosuppression.
The role of prolactin/vasoinhibins in cardiovascular diseases.
Acromegaly
Second line treatment of acromegaly: Pasireotide or Pegvisomant?
Cushing’s
Pregnancy after pituitary surgery does not influence the recurrence of Cushing’s disease.
Spotlight: Dr. Fernandez-Miranda
 This month the PNA Spotlight focuses on Dr. Juan Carlos Fernandez-Miranda, a Professor of Neurosurgery and the Surgical Director of Brain Tumor, Skull Base and Pituitary Centers at Stanford University. Dr. Fernandez-Miranda did a neurosurgery residency at La Paz University Hospital in Madrid, Spain. He completed a fellowship in microsurgical neuroanatomy at the University of Florida. He did clinical training in cerebrovascular surgery at the University of Virginia, and in endoscopic endonasal and open skull base surgery at University of Pittsburgh Medical Center (UPMC). He joined the faculty at Stanford earlier this year. He was kind enough to answer some questions from the PNA. His answers are below:
This month the PNA Spotlight focuses on Dr. Juan Carlos Fernandez-Miranda, a Professor of Neurosurgery and the Surgical Director of Brain Tumor, Skull Base and Pituitary Centers at Stanford University. Dr. Fernandez-Miranda did a neurosurgery residency at La Paz University Hospital in Madrid, Spain. He completed a fellowship in microsurgical neuroanatomy at the University of Florida. He did clinical training in cerebrovascular surgery at the University of Virginia, and in endoscopic endonasal and open skull base surgery at University of Pittsburgh Medical Center (UPMC). He joined the faculty at Stanford earlier this year. He was kind enough to answer some questions from the PNA. His answers are below:
What inspired you to choose your career path?
When I was a young kid, about 10-11 years old, I got sick with a skin rash and high fever; the family doctor visited our home, carefully examined me, and based on a number of clues, he determined I got a very rare bacterial infection known as scarlet fever; a few days of antibiotic medication and I was back to normal. I now realized that I was fascinated by the wisdom, expertise, and detective attitude of the physician, and this personal event was (I now know) key to my future decision to become a doctor.
As I started medical school, I became deeply interested in the structure of the brain and how it explains brain and perhaps even mind function. I realized that the closest I could get to know the brain was actually as a surgeon operating on it.
I became a neurosurgery resident, and I immediately felt that entering into a patient’s brain, skull base, or pituitary gland was a huge privilege and a unique experience that will require my entire devotion and attention. I learned from my mentors the importance of precise knowledge of surgical neuroanatomy to perform gentle, accurate, and safe surgery. After residency training, I decided to spend 2 entire years in the lab – fully dedicated to mastering the understanding of the complex tridimensional surgical neuroanatomy required to safely and efficiently navigate the brain and skull base. These years, under the guidance of legendary neurosurgeon Albert Rhoton, served as the basis of everything I have accomplished thus far.
I was then fortunate to continue my clinical training at University of Virginia with several giants of neurosurgery, and I was greatly influenced by the meticulous approach of Dr. Ed Olfield’s pituitary surgeries, particularly for Cushing’s disease. It was such a joy to watch his precise extracapsular tumor resections. At the same time, I had become totally enchanted by the endoscopic endonasal operations that Dr. Amin Kassam was performing at University of Pittsburgh, and after many requests he finally accepted me for specialized training with him and his team. That was a life changing event for me, as my career was about to be centered in the development and refinement of endoscopic endonasal skull base and pituitary surgery.
What is the primary focus of your work/research?
My primary clinical focus is the treatment of patients with pituitary, skull base, and brain tumors. I have particular technical expertise in endoscopic endonasal surgery for pituitary tumors and other skull base lesions, such as craniopharyngiomas, meningiomas, and chordomas, with an accumulated surgical experience of more than 1,000 cases. My clinical practice includes a full range of minimally invasive approaches, in addition to complex open skull base and brain surgery.
My research interests lie in the study of surgical neuroanatomy and the application of innovative techniques into the operating room that aim to improve surgical safety and effectiveness. As an example, along with my fellows, we have recently provided a new compartmental classification of the cavernous sinus that may help improve resection rates of pituitary tumors that invade the cavernous sinus, while preserving cranial nerve function. We have also described the structure of the medial wall of the cavernous sinus and the ligaments that anchor it to the carotid artery, and we have implemented an innovative surgical technique to selectively remove the medial wall of the cavernous sinus; this is extraordinarily important to achieve complete remission in certain functional tumors causing Cushing’s disease or acromegaly, and our results have proven not only the efficacy of this novel technique, but its safety when appropriately performed.
What do you consider to be the future of your field?
There is no doubt that the field is already moving towards multidisciplinary super-specialization, promoting the creation of Pituitary Centers of Excellence that provide dedicated clinical care, research, and education. This favorable trend will facilitate the development of more effective surgical and medical treatments. Pituitary tumors should only be treated by fellowship-trained neurosurgeons in this field at high-volume surgical centers.
In spite of the multiple advances in the treatment of pituitary tumors, we are still in need of further improvement at all levels. From the surgical point of view, the future is on developing better visualization tools and mini-robotic instruments that will allow more effective and less invasive operations. From the imaging point of view, I believe functional imaging, such as PET-MRI, may improve the diagnosis and localization of hormonally active microadenomas with “negative” MRI studies. The future will hopefully bring newer and more effective medical therapies for active and even inactive pituitary tumors.
What should patients know about your field/what deserves more recognition/awareness?
I think the most important message for current and future patients is to make sure they seek the best team around to treat their disease. It is important to emphasize the team approach, because experience, knowledge, and collaboration is critical to obtaining the best outcome. This extends to all members of the team, including not only the neurosurgeon and the endocrinologist, but also ENT, neuro-ophthalmologist, radiation therapist, neuroradiologist, and neuropathologist.
What would you like to convey about yourself to your patients?
I strive to offer my patients the best possible treatment, that combines ultimate surgical and technological applications with compassionate care. I believe in teamwork and I am privileged to work with such a stellar team at Stanford. I have dedicated my life to becoming the best possible surgeon for my patients.
Why did you get involved with the PNA and what is the extent of your involvement?
I have always been fascinated by the diagnosis and treatment of pituitary tumors and pituitary diseases, and I feel extremely fortunate to dedicate a large portion of my practice to helping pituitary patients. My motivations perfectly align with the PNA goals, and this is the main reason I got involved. I have contributed to the education and counseling of patients through the PNA and I hope to continue to do so for the years to come.
PNA Highlights September 2022

When everything seems to be going against you, remember that the airplane takes off against the wind, not with it.
-Henry Ford
PNA Spotlight: Dr. Edward Laws
This month the PNA Spotlight focuses on Dr. Edward R Laws, MD, FACS, a Professor of Neurosurgery at Brigham and Women’s Hospital (MGB) in Boston/Harvard Medical School. He also serves as Director of the Pituitary/Neuroendocrine Center in the Department of Neurosurgery at Brigham and Women’s Hospital in Boston, Massachusetts. Boston, Massachusetts. Dr. Laws was kind enough to send us a letter about his career in the field of pituitary neurosurgery, which we reprint here in its entirety. Dr. Laws has been an integral part of the PNA since the beginning 30 years ago. We are grateful for his friendship and service.
My medical career began in 1959 as a first-year student at the Johns Hopkins School of Medicine. Among all of the new information and coursework, I quickly developed an interest in the anatomy, pathology, and physiology of the brain, and that interest never went away! In 1960, I was fortunate to have a great mentor for research on the nervous system, giving me a launching point for expanding my research interests to pituitary surgery and endocrinology, which has fully lasted as my favorite topic and source of effort.

Medical Corner: Can Prolactin Protect You?
This month the PNA Medical Corner features an article co-authored by a longtime member of the PNA, Dr. Maria Fleseriu, a Professor of Endocrinology and Neurological Surgery and Director of the Pituitary Center at Oregon Health & Science University. The study looks the the use of the drug osilodrostat for treatment of Cushing’s Syndrome and makes recommendations on best practices.
Treatment of Cushing’s syndrome with osilodrostat: practical applications of recent studies with case examples
Maria Fleseriu , Beverly M K Biller
Affiliations expand
• PMID: 36002784 PMCID: PMC9401199 DOI: 10.1007/s11102-022-01268-2
Abstract

Magnolia
PATHFNDR

Investigational Studies to Evaluate the Safety and Efficacy of Paltusotine in Patients with Acromegaly
The PATHFNDR studies are recruiting patients to participate in clinical research for once-daily paltusotine for the treatment of acromegaly. If the studies are successful, paltusotine could be approved as a ONCE-DAILY, ORAL treatment option that gives patients an alternative to injections or twice-daily oral medications.
As a study participant, you could play an important role in advancing the options available for acromegaly treatment for yourself and many others living with this rare disease.
ABOUT THE STUDIES
The purpose of the PATHFNDR studies is to see if Crinetics Pharmaceutical's investigational medication, paltusotine, is safe and effective in patients with acromegaly.
PATHFNDR-1 is a randomized, placebo-controlled study designed to evaluate the safety and efficacy of paltusotine in
subjects with acromegaly treated with somatostatin receptor ligand (SRL) based treatment regimens. Clinicaltrials.gov
PATHFNDR-2 is a randomized, placebo-controlled study designed to evaluate the safety and efficacy of paltusotine in
subjects with non-pharmacologically treated acromegaly. Clinicaltrials.gov
1(855) 848-8486
Copyright © 2024 Pituitary Network Association All rights reserved.
Disclaimer: PNA does not engage in the practice of medicine. It is not a medical authority, nor does it claim to have medical expertise. In all cases, PNA recommends that you consult your own physician regarding any course of treatment or medication.
Our mailing address is:
Pituitary Network Association
P.O. Box 1958
Thousand Oaks, CA 91358
(805) 499-9973 Phone - (805) 480-0633 Fax
Email [email protected]
You are receiving this Newsletter because you have shown interest in receiving information about our activities.
If you do not want to receive any more emails from PNA, Unsubscribe.
PNA Highlights August 2022

The first wealth is health.
– Ralph Waldo Emerson
Spotlight: Dr. Fernandez-Miranda
This month the PNA Spotlight focuses on Dr. Juan Carlos Fernandez-Miranda, a Professor of Neurosurgery and the Surgical Director of Brain Tumor, Skull Base and Pituitary Centers at Stanford University. Dr. Fernandez-Miranda did a neurosurgery residency at La Paz University Hospital in Madrid, Spain. He completed a fellowship in microsurgical neuroanatomy at the University of Florida. He did clinical training in cerebrovascular surgery at the University of Virginia, and in endoscopic endonasal and open skull base surgery at University of Pittsburgh Medical Center (UPMC). He joined the faculty at Stanford earlier this year. He was kind enough to answer some questions from the PNA. His answers are below:
What inspired you to choose your career path?
When I was a young kid, about 10-11 years old, I got sick with a skin rash and high fever; the family doctor visited our home, carefully examined me, and based on a number of clues, he determined I got a very rare bacterial infection known as scarlet fever; a few days of antibiotic medication and I was back to normal. I now realized that I was fascinated by the wisdom, expertise, and detective attitude of the physician, and this personal event was (I now know) key to my future decision to become a doctor.
Medical Corner: Can Prolactin Protect You?
This month the PNA Medical Corner spotlights an article co-authored by PNA member G. Edward Vates, a professor of neurosurgery at the University of Rochester. The study finds that a moderately high level of prolactin (but not excessively high level) seems to protect retinal function in patients with a tumor squeezing the optic chiasm.
Link: https://pubmed.ncbi.nlm.nih.gov/35921360/
Prolactin at moderately increased levels confers a neuroprotective effect in non-secreting pituitary macroadenomas.
Affiliations expand
• PMID: 35921360 PMCID: PMC9348739 DOI: 10.1371/journal.pone.0271690
Abstract

Magnolia
PATHFNDR

Investigational Studies to Evaluate the Safety and Efficacy of Paltusotine in Patients with Acromegaly
The PATHFNDR studies are recruiting patients to participate in clinical research for once-daily paltusotine for the treatment of acromegaly. If the studies are successful, paltusotine could be approved as a ONCE-DAILY, ORAL treatment option that gives patients an alternative to injections or twice-daily oral medications.
As a study participant, you could play an important role in advancing the options available for acromegaly treatment for yourself and many others living with this rare disease.
ABOUT THE STUDIES
The purpose of the PATHFNDR studies is to see if Crinetics Pharmaceutical's investigational medication, paltusotine, is safe and effective in patients with acromegaly.
PATHFNDR-1 is a randomized, placebo-controlled study designed to evaluate the safety and efficacy of paltusotine in
subjects with acromegaly treated with somatostatin receptor ligand (SRL) based treatment regimens. Clinicaltrials.gov
PATHFNDR-2 is a randomized, placebo-controlled study designed to evaluate the safety and efficacy of paltusotine in
subjects with non-pharmacologically treated acromegaly. Clinicaltrials.gov
1(855) 848-8486
Copyright © 2024 Pituitary Network Association All rights reserved.
Disclaimer: PNA does not engage in the practice of medicine. It is not a medical authority, nor does it claim to have medical expertise. In all cases, PNA recommends that you consult your own physician regarding any course of treatment or medication.
Our mailing address is:
Pituitary Network Association
P.O. Box 1958
Thousand Oaks, CA 91358
(805) 499-9973 Phone - (805) 480-0633 Fax
Email [email protected]
You are receiving this Newsletter because you have shown interest in receiving information about our activities.
If you do not want to receive any more emails from PNA, Unsubscribe.
News Articles September 2022
Mother Fights to Get School Staff Trained on Pituitary Injections
A mother in the U-K is working to get training for staff at her daughter’s school, so they can give her an emergency injection. The girl suffers from panhypopituitarism and may require a hydrocortisone injection in an emergency situation. But the school will not authorize it staff to administer an intramuscular injection without proper training. Liability issues are at the heart of the matter. Now the mother is petitioning the government to step in. Read more:
Signs of a Hormonal Imbalance
An article in Health Digest gives an exhaustive rundown of all the possible signs of a hormonal imbalance, including unusual body odor. Read more:
Cushing’s and Job Stress: A Personal Story
Paris Dancy’s latest column in Cushing’s Disease News follows his career struggles as he battled Cushing’s. Read more:
A Mother Uses Positive Affirmation Chants to Help Daughter with Pituitary Issues
A story on the Upworthy website tells the story of a mother who chants positive affirmation to her young daughter, who is blind and has an underdeveloped pituitary. Read more:
Patient story: Teen Excels in School Despite Pituitary Tumor
A story in the Derbyshire Times follows the case of a teen girl there named Deeti Wren, who underwent surgery for a pituitary brain tumor, and carried on with her studies anyway, managing to take her GSCE’s despite the health troubles. Read more:
FSH, Obesity, and Breast Cancer
Researchers at the University at Buffalo and the University of Arizona are studying the role of Follicle-Stimulating Hormone (FSH) in obesity. Obesity is a risk factor for breast cancer, so they are looking for a through-line from obesity to excess FSH to breast cancer. Read more:
News Articles August 2022
Chinese Cancer Researchers Study Pituitary Hormone Receptors
The Journal Science reports that researchers with the University of Science and Technology of China “have made a breakthrough in the treatment of cancer through immunotherapy, identifying a particular hormone receptor as a potential target for the treatment.” The receptor promotes tumor growth. It is called MC5R and works with the pituitary hormone α-MSH which is produced by the pituitary gland. Read More:
Son Grows Hair, Makes a Wig for Mom with Pituitary Tumor
 The Today Show’s website has the story of a man in Arizona who grew out his hair for two years in order to make a wig for his mother, who suffers from a recurring pituitary tumor. Read more:
The Today Show’s website has the story of a man in Arizona who grew out his hair for two years in order to make a wig for his mother, who suffers from a recurring pituitary tumor. Read more:
Caption: Melanie and Matt Shaha (Courtesy Shaha family.)
Study: Signifor Reduces Tumors in Cushings
An article in Cushing’s Disease News looks at research that found that SignifActor With Acromegaly Passes Away In Los Angelesor reduced tumor size in 40% of Cushing’s patients in the study, but most of them had already had surgery. Read more:
Symptoms of a Brain Tumor
An article in VeryWellHealth lists the common signs of a brain tumor: “vomiting, seizures, balance problems, dizziness, personality changes, loss of consciousness, and more.”
Read more:
Well-Known Egyptian Acromegalic Dies at Age 27
The PNA sends its condolences to the family of Huda Abdel-Gawad, a 27-year-old acromegalic who passed away recently from kidney failure. Abdel-Gawad had come to be known as Egypt’s tallest woman. Read more:
Actor With Acromegaly Passes Away In Los Angeles
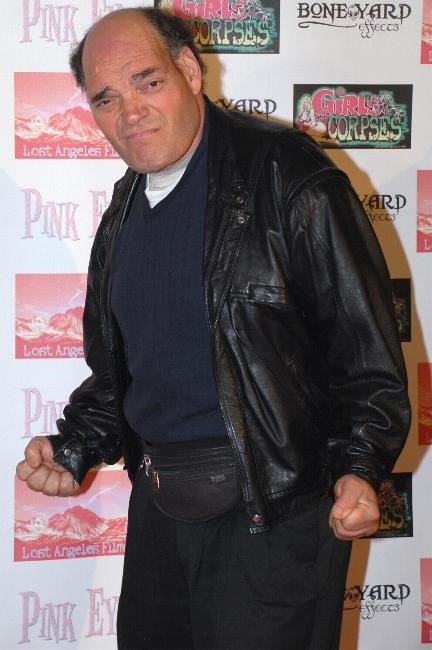 Character actor Irwin Keyes passed away recently at age 63 from complications of acromegaly. He was known for his roles in “House of 1000 Corpses”, “The Jeffersons” and “Intolerable Cruelty”.
Character actor Irwin Keyes passed away recently at age 63 from complications of acromegaly. He was known for his roles in “House of 1000 Corpses”, “The Jeffersons” and “Intolerable Cruelty”.
Caption: Actor and acromegalic Irwin Keyes. (Wikimedia Commons)
PNA Medical Corner: Incipient Gigantism
This month the PNA Medical Corner highlights an article co-authored by Dr. Albert Beckers, a longtime member of the PNA. The study looks at the case of a 7-year-old boy with a pituitary tumor due to a gene mutation. They conclude that not all tumors of this type respond to pasireotide.
AACE Clin Case Rep
. 2021 Dec 16;8(3):119-123.
doi: 10.1016/j.aace.2021.12.003. eCollection May-Jun 2022.
• PMID: 35602875 PMCID: PMC9123570 DOI: 10.1016/j.aace.2021.12.003
Abstract
Background: Our objective was to describe the clinical course and treatment challenges in a very young patient with a pituitary adenoma due to a novel aryl hydrocarbon receptor-interacting protein (AIP) gene mutation, highlighting the limitations of somatostatin receptor immunohistochemistry to predict clinical responses to somatostatin analogs in acromegaly.
Case report: We report the case of a 7-year-old boy preventing with headache, visual field defects, and accelerated growth following failure to thrive. The laboratory results showed high insulin-like growth factor I (IGF-I) (standardised deviation scores ( +3.49) and prolactin levels (0.5 nmol/L), and magnetic resonance imaging identified a pituitary macroadenoma. Tumoral/hormonal control could not be achieved despite 3 neurosurgical procedures, each time with apparent total resection or with lanreotide or pasireotide. IGF-I levels decreased with the GH receptor antagonist pegvisomant. The loss of somatostatin receptor 5 was observed between the second and third tumor resection. In vitro, no effect on tumoral GH release by pasireotide (with/without cabergoline) was observed. Genetic analysis revealed a novel germline AIP mutation: p.Tyr202∗ (pathogenic; class 4).
Discussion: In vitro response of tumor tissue to somatostatin may better predict tumoral in vivo responses of somatostatin analogs than somatostatin receptor immunohistochemistry.
Conclusion: We identified a novel pathologic AIP mutation that was associated with incipient acrogigantism in an extremely young patient who had a complicated course of disease. Growth acceleration can be masked due to failure to thrive. Tumoral growth hormone release in vivo may be predicted with in vitro exposure to somatostatin receptor analogs, as it cannot be assumed that all AIP-mutated somatotropinomas respond well to pasireotide.
Keywords: AIP mutation; AIP, aryl hydrocarbon receptor–interacting protein; GH, growth hormone; IGF-I, insulin-like growth factor I; LAR, long-acting release; NR, normal range; SDS, standardised deviation scores; SSA, somatostatin analog; SSTR, somatostatin receptor; acromegaly; gigantism; macroadenoma; pituitary adenoma; somatotropinoma.
PNA Spotlight: Dr. Luma Ghalib
 This month’s PNA Spotlight shines on Luma Ghalib, MD, F.A.C.E., a professional member of the PNA and an esteemed endocrinologist at The Ohio State University. Dr. Ghalib attended medical school at Baghdad University and completed a residency in internal medicine at Medical City Teaching Hospital in Baghdad. She then moved with her husband to New Zealand, where she did her initial training at Auckland Healthcare. She did a second residency in internal medicine at the Medical College of Ohio. Dr. Ghalib finished her endocrinology fellowship training at Chicago Medical School, part of Rosamund Franklin University. She then worked with Mary Washington Healthcare in Virginia as a consultant endocrinologist. Dr. Ghalib joined The Ohio State University in 2013 and she worked closely with neurosurgery and the ENT team to create a state-of-the-art Skull Base and Pituitary Clinic. She is currently an Assistant Professor in the Division of Endocrinology, Diabetes and Metabolism at The Ohio State University. She was kind enough to answer some questions from the PNA:
This month’s PNA Spotlight shines on Luma Ghalib, MD, F.A.C.E., a professional member of the PNA and an esteemed endocrinologist at The Ohio State University. Dr. Ghalib attended medical school at Baghdad University and completed a residency in internal medicine at Medical City Teaching Hospital in Baghdad. She then moved with her husband to New Zealand, where she did her initial training at Auckland Healthcare. She did a second residency in internal medicine at the Medical College of Ohio. Dr. Ghalib finished her endocrinology fellowship training at Chicago Medical School, part of Rosamund Franklin University. She then worked with Mary Washington Healthcare in Virginia as a consultant endocrinologist. Dr. Ghalib joined The Ohio State University in 2013 and she worked closely with neurosurgery and the ENT team to create a state-of-the-art Skull Base and Pituitary Clinic. She is currently an Assistant Professor in the Division of Endocrinology, Diabetes and Metabolism at The Ohio State University. She was kind enough to answer some questions from the PNA:
What inspired you to choose your career path?
I wish I had a fancy story to share, but I admit I followed my older sister’s path to become a physician and start medical school. Once I started my clinical rotation and got to talk to patients and their families, I knew that was where I wanted to spend the rest of my career. Picking endocrinology was easy. It is so logical and follows precise pathways that can be understood if you look hard and connect the dots. The pituitary gland makes most of the body’s hormones, which makes pituitary disease more challenging but also more rewarding to treat.
What is the primary focus of your work/research?
We handle a variety of cases in the comprehensive multidisciplinary Pituitary – Skull Base Clinic at the Ohio State University. We have a high volume of patients with malignant and benign lesions in the sellar area at the James Cancer Hospital. I work closely with neurosurgery, neuro- oncology, neuro-ophthalmology and ENT teams to provide comprehensive care for the patients and their families. The center has been involved with multiple trials evaluating the efficacy and safety of emerging treatments for Cushing’s and acromegaly.
What do you consider to be the future of your field?
There are several interesting and exciting treatments in the pipeline for functioning pituitary adenomas like Cushing’s and acromegaly. Cracking the genetic code, mutations will be the next big thing coming down the pike. I know we are not there, yet. But working at the James Cancer Hospital with my oncology colleagues, and seeing the advances in the oncology world – nothing seems impossible.
What should patients know about your field/what deserves more recognition/awareness?
Working in a big center makes me forget at times how rare some of the pituitary diseases are. We take care of patients who struggled for years before someone thought about the possibility of a pituitary-related illness. I believe that knowledge is power and it is great to be your own advocate. Many of the symptoms can be vague, slowly progressive and can be easily misdiagnosed.
Educating patients is great, but it is just as important to raise awareness in the medical community, which is comprised of people with different backgrounds. I take every opportunity to teach our medical students and residents what to expect and what to look for.
What would you like to convey about yourself to your patients?
It is my privilege to take care of them. They teach me as much as I teach them. By sharing their stories and struggles, they open my eyes to how many different ways the same illness can present. As we say here at the Ohio State University, no two people are the same.
Why did you get involved with the PNA and what is the extent of your involvement?
I have to thank my neurosurgery colleague Dr. Prevedello, who introduced me to the PNA many years ago. Since then, I try to keep active with a great, fun team at the PNA. I have presented webinars and answered members’ questions when needed. I am looking forward to working with the team to have another pituitary symposium at the Ohio State University in the future.
PNA Medical Corner: Quality of Life for Acromegalics
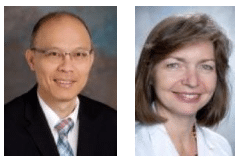 This month the PNA Medical Corner focuses on an article co-authored by two members of the PNA, Drs. Kevin Yuen and Ursula Kaiser. The study compared the quality of life for groups of acromegaly patients; one that received pharmacological therapy, the other that did not. They conclude that acromegalics who develop growth hormone deficiency have lower quality of life. They found that while pharmacologic or radiotherapy don’t lower a person’s quality of life, their overall quality of life is suboptimal despite biochemical control.
This month the PNA Medical Corner focuses on an article co-authored by two members of the PNA, Drs. Kevin Yuen and Ursula Kaiser. The study compared the quality of life for groups of acromegaly patients; one that received pharmacological therapy, the other that did not. They conclude that acromegalics who develop growth hormone deficiency have lower quality of life. They found that while pharmacologic or radiotherapy don’t lower a person’s quality of life, their overall quality of life is suboptimal despite biochemical control.
Pituitary. 2022 Apr 27.
doi: 10.1007/s11102-022-01224-0. Online ahead of print.
PMID: 35476257 DOI: 10.1007/s11102-022-01224-0
Abstract:
Purpose: To assess long-term quality of life (QoL) in patients with sustained biochemical control of acromegaly, comparing those receiving vs not receiving pharmacotherapy (primary analysis); to assess change in QoL over time (secondary analysis).
Methods: Cross-sectional study, with a secondary longitudinal component, of 58 patients with biochemically controlled acromegaly. All had participated in studies assessing QoL years previously, after having undergone surgery ± radiotherapy. One cohort received medical therapy [MED (n = 33)]; the other did not [NO-MED (n = 25)]. QoL was assessed by the 36-Item-Short-Form Health Survey (SF-36), Acromegaly Quality of Life Questionnaire (AcroQoL), Gastrointestinal Quality of Life Index (GIQLI), Symptom Questionnaire, and QoL-Assessment of Growth Hormone Deficiency in Adults (QoL-AGHDA).
Results: Mean (± SD) duration of biochemical control was 15.0 ± 6.4 years for MED and 20.4 ± 8.2 years for NO-MED (p = 0.007). 58% of subjects scored < 25% of normal on ≥ 1 SF-36 domain and 32% scored < 25% of normal on ≥ 4 of 8 domains. Comparing MED vs NO-MED and controlling for duration of biochemical control, there were no significant differences in QoL by SF-36, AcroQOL, GIQLI, Symptom Questionnaire, or QoL-AGHDA. Growth hormone deficiency (GHD) but not radiotherapy predicted poorer QoL. In MED, QoL improved over time in three AcroQoL domains and two GIQLI domains. In NO-MED, QoL worsened in two SF-36 domains and two Symptom Questionnaire domains; QoL-AGHDA scores also worsened in subjects with GHD.
Conclusion: A history of acromegaly and development of GHD, but not pharmacologic or radiotherapy, are detrimental to QoL, which remains poor over the long-term despite biochemical control.
Keywords: Acromegaly; Growth hormone deficiency; Quality of life; Radiation therapy.
© 2022. The Author(s), under exclusive licence to Springer Science+Business Media, LLC, part of Springer Nature.
PNA Spotlight: Dr. Jamie Van Gompel
 This month the PNA Spotlight focuses on Dr. Jamie Van Gompel with the Mayo Clinic in Rochester, New York. There he serves as Professor in Neurosurgery and Otolaryngology; Assistant Program Director of Neurosurgery Residency; and consultant in the departments of neurosurgery and otorhinolaryngology.
This month the PNA Spotlight focuses on Dr. Jamie Van Gompel with the Mayo Clinic in Rochester, New York. There he serves as Professor in Neurosurgery and Otolaryngology; Assistant Program Director of Neurosurgery Residency; and consultant in the departments of neurosurgery and otorhinolaryngology.
Dr. Van Gompel started out at the University of Wisconsin with a Bachelor of Science degree in biochemistry, medical microbiology and immunology. He then proceeded to earn his M.D. there as well. He went on to complete a certificate program in clinical and translational research at the Mayo Clinic. He then did a fellowship in skull base and complex cranial surgery at the University of South Florida. He was kind enough to answer a series of questions from the PNA. Here are his answers:
• What inspired you to choose your career path?
I am not sure where my fascination with the pituitary gland started, but when I became interested in medicine, I knew I wanted to operate on the endocrine access. Dr. Chen, a huge influence in my life, was chief of endocrine surgery at the University of Wisconsin. He was my primary mentor in medicine and showed me how complicated endocrine surgery could be. I was so fascinated that operating in one part of the body could affect another part so much, as we see in the pituitary gland. Later, we worked with MEN1 mutations in his lab, which I found quite interesting. Fast forward to my work at the Mayo Clinic, the institution in which arguably thyroid hormones were first described and where cortisol was discovered – and where one of the greatest pituitary surgeons of all time – Dr. Ed Laws – started his career, I could not help but be seduced by the field of pituitary surgery. I was fortunate to train with excellent pituitary surgeons of high volume who brought endoscopic pituitary surgery to the Mayo Clinic. Every day I find that something in my life confirms my sincere interest in pituitary surgery.
• What is the primary focus of your work/research?
My focus is on clinical outcomes in pituitary surgery. I try to enhance my craft by performing surgery in a way that is accurate, safe, and gentle while preserving as much normal anatomy as I can. Therefore, I feel that anatomical research is extremely important. However, I realize that, as the primary consult for intervention, it is critical that I recognize that medical alternatives are important as well. They should be considered, because they have the potential to preserve patient well-being and quality of life while treating the patient’s symptoms. As a real life example, we were one of the first institutions to treat Brafv600E papillary craniopharyngiomas with medical treatments. While I acknowledge that the concept was pioneered by the group in Boston, after the first case report appeared we adopted this method quickly. We supported the research because it was the right thing to do for the patient.
• What do you consider to be the future of your field?
The future of our field is to continue to pursue excellent outcomes with surgery. Hopefully with some of the more difficult tumors (that are not surgically curable like large growth hormone-secreting tumors involving the cavernous sinus) we can help our patients by finding treatments that complement or obviate surgery.
• What should patients know about your field/what deserves more recognition/awareness?
Although all surgeries are scary, most patients do very well after pituitary surgery with minimal complications. It is critical to have your first surgery with a surgeon who has experience and does the procedure routinely (more than 50 transsphenoidal procedures per year) to ensure you can maximize your surgical outcome on the first operation. This gives you the best chance of avoiding a second surgery or an adjuvant treatment, like radiation.
• What would you like to convey about yourself to your patients?
I do more than 100 pituitary procedures a year, and address not only tumors of the pituitary gland but also conditions that involve areas around the pituitary gland, such as the cavernous sinus and optic nerves. In my opinion, a surgeon should not solely think about the approach, but also about the patient outcome. The surgeon should be well-versed in open and endoscopic procedures in order to understand the nuances that lead to excellent patient outcomes.
• Why did you get involved with the PNA and what is the extent of your involvement?
I got involved with the PNA because it is a critical resource for patients to have an unbiased patient-centered resource to provide information valuable to those in their most critical times of need. The PNA attempts to bring those interested in treating the disease together with those suffering from the disease. I hope to ease patient suffering by being involved with the PNA.
Available Now!
The Pituitary Patient Resource Guide Sixth Edition is now available! Be one of the first to have the most up-to-date information. The Pituitary Patient Resource Guide a one of a kind publication intended as an invaluable source of information not only for patients but also their families, physicians, and all health care providers. It contains information on symptoms, proper testing, how to get a diagnosis, and the treatment options that are available. It also includes Pituitary Network Association's patient resource listings for expert medical care.

Xeris Pharmaceuticals is valued member of the PNA