News Articles February 2022
Written on 04 February 2022.
Symptoms of a Pituitary Disorder
Symptoms of a Pituitary Disorder
Do you or a loved one suffer from undiagnosed symptoms? Do you go from doctor to doctor trying to find out why you feel so bad only to be told that there is nothing wrong with you, it’s all in your head? It may be all in your head, your symptoms may be caused by your pitiutary gland. For detailed information about the pituitary gland visit our about pituitary section.
The pituitary gland is often referred to as the “Master Gland” of the body. Due to the pituitary’s involvement in regulating hormones, any pituitary disturbance can create a hormonal imbalance. Hormonal imbalances can cause a number of symptoms, some of which are listed below.
- Headaches
- Depression
- Mood/Emotion Swings
- Anger
- Loss of Memory
- Loss of Sleep
- Sexual Dysfunction
- Lethargy
- Weakness in Limbs
- High Blood Pressure
- Unusual Hair Growth
- Eating Disorders
- Anorexia
- Obesity
- Bulimia
- Weight Gain
- Diabetes
- Infertility
- Impotence
- Irregular Menses
- Lactating
One or more of these symptoms may not indicate a pituitary disorder, but if you have some of these and they are unexplained, you owe it to yourself to investigate further. Take the time to go through the important information here on the PNA Website. Ask your physician about all your symptoms. Often symptoms are dealt with as individual pieces, without a look at the whole puzzle. When that happens the symptom is treated, but not the underlying cause.
Research and Facts
“1 in 5 individuals may have an abnormal growth on their pituitary gland, causing significant health complications that, if left undiagnosed and untreated, can impair normal hormone function and result in a reduced lifespan.”
Shereen Ezzat, M.D., Professor of Medicine, University of Toronto
Some have estimated nearly 30%. In reviewing dozens of studies over the past 80 years on the Prevalence of Pituitary Tumors, the consensus was reached that at least 16.7% of the population develop or harbor pituitary tumors. Supported by the PNA and published by the American Cancer Society June 2004, the systematic review abstract “The Prevalence of Pituitary Adenomas.
PDF full text file available here Prevalence_Of_Pituitary_Adenomas.pdf
Take the First Three Steps
Step 1: Take action and get educated. Knowledge is Power!
WHAT IS THE PITUITARY GLAND AND WHAT DOES IT AFFECT?
The pituitary is a small, pea-sized gland located at the base of the brain that functions as “The Master Gland.” From its lofty position above the rest of the body it sends signals to the thyroid gland, adrenal glands, ovaries and testes, directing them to produce thyroid hormone, cortisol, estrogen, testosterone, and many more. These hormones have dramatic effects on metabolism, blood pressure, sexuality, reproduction,and other vital body functions. In addition, thepituitary gland produces growth hormone for normal development of height and prolactin for milk production.
For more information visit the “About Pituitary” page.
Visit our online bookstore at www.pituitarybooks.com for valuable resources to educate yourself on the latest information and the best treatments available.
Purchase the Pituitary Patient Resource Guide Fifth Edition from www.pituitarybooks.com. This amazing guide will give you a wealth of information on everything from symptoms and diagnosis to treatment and surgery options. Included is a list of Pituitary Health Care Providers and Pituitary Treatment Centers. You owe it to yourself to make sure that you are armed with the power to obtain the best quality of life possible.
Step 2: Join the Pituitary Network Association
The PNA is dedicated to providing valuable information to pituitary patients worldwide. We strive on a daily basis to find relevent, reliable information that patients can trust. There is so much misinformation available on the internet. The PNA Staff, along with it’s panel of Scientific Advisors, seeks out information you can trust about the latest findings. The PNA commissions studies about pituitary related illnesses and disorders. The PNA puts together Resource Guides and other publications geared toward educating not only patients, but physicians as well. The PNA provides webinars presented by some of the top Pituitary Care Providers in the world to provide information about pituitary disorders, including how to diagnose and treat them. These webinars are viewed worldwide by patients, their families, physicians and mental health care providers.
Becoming a member supports these efforts. No other organization provides this level of information and support. Since we are a nonprofit organization we operate on membership fees, donations and grants. Without members we will not have the ability to provide all of these services for patients. Being a PNA member allows you exclusive access to our library of previous webinars and access to our Ask the Experts program.
Step 3: Explore this website
Until the day comes when it’s common for pituitary disorders to be properly diagnosed and treated by family physicians and specialists, it’s up to YOU to become actively involved in this process. The PNA website offers a wealth of information to you. You’ll find news of the PNA’s efforts, articles on the latest studies, links to successful treatment centers, forums where you can compare notes with other pituitary patients, reports from physicians on the leading edge of research and treatment, a bookstore loaded with invaluable resources, and much more – all continually updated.
Finding the Right Doctor
As of now, few criteria exist for evaluation of physicians and their experiences with pituitary issues in general and tumors inparticular. The PNA, with the help of doctors and patients experienced with pituitary diseases and tumors, has compiled this list of simple, straight forward questions.
Ask these questions of your current physician to help confirm your comfort level with him/her. Take a copy of this list when looking for a new doctor to treat you. Decide what answers you will accept and which ones are automatic red flags. If at all possible, bring your spouse or friend to keep notes and help you stay focused on the medical interview(s). Remember, YOU ARE INCHARGE OF YOUR OWN CARE. YOU HAVE THE FINAL VOTE. Take care of yourself first.
The following two questions should be answered before you visit the doctor. The information is available from your state’s Medical Association.
- Is the doctor Board Certified in his/her field of specialty?
- Where did he/she receive training?
For the Endocrinologist:
- Do you have many patients with my type of problem? How many?
Since there are many types or varieties of pituitary tumors, no specific answer can be expected. If the physician has seen many patients with this problem, then that is a positive sign. However, it gives no insight into the quality of their experience.
- Do you specialize in pituitary tumors and disease?
There are many areas of endocrinology. You want a pituitary specialist.
- Do you have a neurosurgical colleague that you routinely refer patients to?
It is generally encouraged that an endocrinologist would develop a relationship with one or several neurosurgeons that would be able to discuss the evaluation, decision making and post operative treatment.
- Do your neurosurgical colleagues routinely refer pituitary patients to you for pre- and post-operative management?
It is highly desirable that a neurosurgeon work with an endocrinologist before and after surgery to assure the intervention decision is correct, that the patient is well prepared for surgery, and that the patient has post-operative endocrine assessment which helps ensure proper post-operative treatment. In general, it is recommended that endocrinologists handle the long term follow-up of a patient with pituitary disease.
- How do you usually treat patients with my problem?
Does the doctor treat with medication first before resorting to surgery or radiation, or does he/she use combined approaches?
- How will my hormone levels influence your decision on treatment of my pituitary tumor?
No patient with a pituitary adenoma should go to surgery without a pituitary hormone level baseline test being done and a decision made as to whether medical or surgical treatment would be most appropriate. Decisions would be based upon the individual circumstances. In general, however, there is an increasing trend to treat these tumors with drugs to shrink the tumor mass. In many instances this is used as primary treatment, with surgery only after drug therapy fails to bring about the desired tumor shrinkage.
For the Neurosurgeon:
- Do you specialize in pituitary surgery?
- How many pituitary surgeries do you perform every week/month/year?
There is reason to believe that 2 – 5 operations per month are the minimum for a neurosurgeon to perform to maintain a high degree of surgical competency.
- Do you always treat patients with prolactin secreting macroadenomas with surgery?
No patient with a pituitary adenoma should go to surgery without a pituitary hormone level baseline test being done and a decision made as to whether medical or surgical treatment would be most appropriate. Decisions would be based upon the individual circumstances. In general, however, there is an increasing trend to treat these tumors with drugs to shrink the tumor mass. In many instances this is used as primary treatment, with surgery used only if drug therapy fails to bring about the desired tumor shrinkage.
- To whom do you refer patients for pre- andpost-operative management?
It is highly desirable that a neurosurgeon work with an endocrinologist especially before and after surgery to assure that the intervention decision is correct, that the patient is well prepared for surgery, and that the patient has post-operative endocrine assessment which helps ensure proper post-operative treatment.
- On an annual basis, what are the outcomes of your surgeries?
Morbidity? (Complications)
Outcome? (Chemical cure/total resection, remission, etc.)
For the Radiation Physician:
How many pituitary tumors do you treat each year?
What planning system do you have?
Is it based on CT or MRI?
Why do you recommend Radiosurgery rather than Conformal or Conventional Fractionated Radiotherapy? (these terms are interchangeable depending on what is recommended)
What methods are available at your institution?
What is the cost, and how does it compare with the other methods?
What are the risks?
A. Lack of control of tumor
B. Visual damage
C. Secondary tumor development
D. Intellectual impairment
E. Pituitary hypothalamic failure
What are your results?
A. Control of tumor growth
B. Normalization of the hormonal hypersecretion
C. What complications may occur in my specific case?
Questions for ANY physician:
- What written information do you provide to patients with my problem?
- Where do you refer them for additional information?
- Are there new approaches to treatment of my pituitary problem? How did you hear about them?
Is the doctor keeping up on things? There may or may not be new approaches but the response can give you a comfort level that the doctor is keeping up. Ideally, his/her information would come from literature or medical meetings, not from a pharmaceutical company representative alone.
- May I speak to some of your other patients with similar problems?
He/She should have other patients willing to talk about their experiences and results.
- What is the best scan to see a pituitary tumor?
It is generally acknowledged that an MRI is much more effective in assessing a pituitary mass lesion than a CAT scan. A physician that is not aware of that would not be experienced in dealing with pituitary tumors.
- Where and under what circumstances to you refer patients for radiology?
- Psychological counseling?
- Other specialists?
The PNA believes that patient care must include interdisciplinary management of the patient’s problems.
Pituitary/Hormonal Difficulties: Signs and Symptoms and What to Ask Your Physician
Symptoms
Often individual symptoms get treated in today’s world, not underlying causes. If many of the following are present and are significant to you, talk with your doctor or find a doctor who is qualified to pursue further evaluation. Qualified physicians can be found in the medical resources section of this website.
- Headaches, particularly with a sudden onset and in the center of the head
- Sexual difficulties (painful intercourse, low libido, erectile dysfunction)
- Depression and/or changes in mood (anger, depression, anxiety), “bipolar” diagnosis
- Recent and or sudden onset of family, friend relationship difficulties in conjunction with physical symptoms on this list including loss of relationships resulting in isolation, loneliness
- Infertility
- Growth abnormalities/changes especially of the hands (large fingers), feet, head, jaw and separation of teeth
- Obesity (especially in the central area of the body), especially weight gain over a short time, rounding or “moon face”, a large bump/hump on the back on the neck/back. Note: if you suddenly are unable to manage your weight with proper diet and increased activity/exercise, this is a hormonal red flag.
- Eating disorders: excessive weight loss, gain, bulimia. (loss of interest in food or uncontrollable urges to eat)
- Vision changes including loss of peripheral vision, blurring etc. especially with sudden onset
- Skin thinning, stretch marks, bruising easily, acne and cuts or abrasions/pimples that don’t seem to heal
- Carpel tunnel syndrome
- Menstrual difficulties (irregular periods, discontinued, painful, no ovulation, anything not usual for your cycle), early menopause
- Fatigue, weakness in the limbs, general muscle weakness
- Hypertension
- Arthritis, aching joints, osteoporosis
- Loss of sleep, changes in sleep cycle
- Memory impairments, poor concentration
- Unusual hair growth (on chest, face etc.) or hair loss (falling out in clumps)
- Skin and hair that becomes extremely dry, scaly and discolored.
- Lactation not associated with pregnancy (breast leakage…even for men)
- History of emotional/physical trauma and/or chronic stress
- Depersonalization i.e. feeling detached from one’s own body/mind
Remember
No one symptom is indicative of a Pituitary tumor but it is important to investigate further and to TRUST your own body/intuition. Some of the above symptoms or a combination of symptoms without an obvious underlying cause should prompt further questioning. Continue to ask medical/mental health professionals until you feel satisfied. Keep a log/record of your symptoms and keep a log of when your symptoms developed. Ask your family, friends if they notice any changes or differences in your behavior or looks. Share your notes and observations with your doctors and mental health professionals. (or purchase a Patient Resource guide from PNA which has a wonderful patient manual for tracking self care, appointments, symptoms and treatments)
If
You suspect a problem you need to specifically ask your doctor for the following medical tests (and ask for exact results not normal/not normal):
- ACTH
- Cortisol
- Estradiol (E2) Extract/Testosterone
- GH
- FSH
- LH
- Prolactin
- Somatomedin-C (IGF-1)
- PSA (males)
- Free T3
- Free T4
- Total T4
- TSH
- 24 Hour urine FREE Cortisol (ideally 3 or more tests to rule-out error or hormone cycling)
Then
If test results show problems, or if the results are within “normal” ranges but you still have symptoms and are not getting answers you trust then you must be seen by a physician who specializes in pituitary tumors and hormonal disturbances (Pituitary Endocrinologist, Pituitary Neurosurgeon etc.). Such doctors are listed on the PNA website.
A mental health professional may also be able to assist you and your family as you go through the struggle of medical tests and dealing with the symptoms. It is important to find a professional who has some understanding of your physical state, specialized training, and/or willingness to learn about Neuroendocrine disorders.
Okay..Now Where Do I Start?
By Robert Knutzen, MBA
And Annie Hamilton
Pituitary Network Association
Many of you are newbies to pituitary/hormonal disease and find yourselves in the same boat most us were rowing just a short time ago. We have attempted to shortcut the search for answers on most aspects of your diagnosis, treatment and lifetime follow-up care. There are three very distinct but equally important aspects to being a hormonally-challenged patient. Dealing with the medical community is interesting and sometimes confusing. The presence of a tumor takes on an overriding importance to some physicians. However, your quality of life may be severely compromised, not by the tumor or its removal, but by your doctor’s failure to monitor your hormone replacement. You need proper medication in carefully measured doses, appropriately spaced check-ups and, very often, professional mental health care. This organization aims to help you land on your feet. We don’t believe it is in your or your family’s best interest to spend the rest of your life living on disability insurance or on other public assistance. You deserve to be well and whole, and it is possible with determination.
By now you may have read and heard so many conflicting estimates of the rarity or severity of pituitary disorders and tumors, that it can be very difficult to discern the truth. The Pituitary Network Association has, since its founding, attempted to distinguish fact from fiction. We have even commissioned a study by some of the world’s leading endocrinologists, neurosurgeons, pathologists and medical mathematicians/statisticians to arrive at a reasonable, recognized starting place. “The Prevalence of Pituitary Adenomas, a Systematic Review,” by Shereen Ezzat, MD at the University of Toronto; Sylvia Asa, MD, Ph D. at the University of Toronto; William Couldwell, M.D. at the University of Utah; Charles E. Barr, M.D., M.B.A., at Roche Laboratories, Inc.; William E. Dodge, M.S., MBA; Mary Lee Vance M.D. at the University of Virginia; and Ian McCutcheon, M.D. at the University of Texas, does exactly that. We DO have the answers and no valid evidence exists to the contrary.
This study was supported by the Pituitary Network Association, and published by the American Cancer Society in June 2004.
In reviewing dozens of studies over the past 80 years on the prevalence of pituitary tumors alone, (not counting Addison’s disease, Sheehan’s syndrome, inflammations, enlargements, etc.) our experts reached a consensus: at least 16.7% of the population develops or harbors pituitary tumors. Some have estimated nearly 30% of the population. (But, as we say here, it’s 1 in 5.) The clinical significance of many of these tumors is the only major issue that divides the true experts. Clinical significance, however, only reflects what individual doctors find to be significant (which does not mean it’s accurate). If your own doctor, for instance, does not believe that headaches, mood swings, apathy, mental/emotional disorders or sexual disorders/dysfunction are related to pituitary tumors, he or she may classify your tumor as clinically insignificant and therefore to discount it. To us as patients, after nearly 15 years of interacting with hundreds of thousands of other patients – that is hardly an acceptable conclusion. All pituitary tumors, in the absence of clear and absolute proof of another medical cause for the patient’s discomfort, must be viewed as significant.
We share some patients’ information with various world experts in medicine, and we collect and read the experts’ opinion and findings from around the world. Yes – headaches, joint pain, mental/emotional disorders, sexual dysfunction, and eating disorders are very often related to pituitary tumors/hormonal disorders. The overwhelming numbers of pituitary patients are not hypochondriacs nor are they “crazy”. Sick? Yes. In need of expert care? Yes. Can they improve their quality of life? Yes. Will they live? Certainly.
The Diagnosis
Getting a correct diagnosis is critical and too often very difficult. Pituitary medicine is the “miracle” branch of hormonal health care. It is hard to believe, but the small, non-functioning tumors deemed clinically insignificant by the uninformed, often will, in a very few months or years, “miraculously” turn into Cushing’s disease, acromegaly or something else. Usually to the patient’s detriment, often causing irreversible damage. Nearly always, this happens due to an incorrect diagnosis, resulting in incorrect treatment, by someone who didn’t take the time to be curious enough.
As a rule, always get, at minimum, a second opinion. Without exception, the opinions must be from experts. In other words; a general practitioner/run of the mill doctor probably isn’t a pituitary expert. They may wear a white lab coat and have an MD but they probably don’t specialize in the right field of health care. Never deviate from this rule. It will come back to haunt you.
For patients and their families and friends, pituitary disease is much like watching a slow-moving train wreck – one that your average doctor seems either indifferent to or incapable of preventing, understanding and treating appropriately. For that reason, you alone must take responsibility for finding the right doctor, and receiving the correct medical diagnosis. You must be persistent, informed, polite and determined. Opinions rendered by non-pituitary related medical experts should be viewed with skepticism and warrant a second or third opinion. If you are among those who prize convenience, and feel you must see a doctor, any doctor, close to home, you probably aren’t ready for the journey necessary for treatment.
Both on our web site www.pituitary.org and other places in this book, you will find the signs, symptoms and even the tests needed to correctly diagnose your disorder. There is no alternative to reading up on yourself; only you know yourself!
Do not try to be your own doctor, but be aware that a physician who is worth his or her salt appreciates working with a well-informed and cooperative patient who shows every sign of wanting to get well, asks questions and listens to the input given.
Try to not get discouraged, and never give up. The average time between onset and diagnosis for a pituitary patient is extraordinarily long. With your help we will create sufficient awareness in the medical community and the public to reduce this time from an average of about seven years to one or two! Practitioners normally use the term “benign” to differentiate non-cancerous from cancerous tumors. This does not necessarily mean harmless or of little importance. It may not be your tumor that kills you -it may be any one of a hundred disorders, from cancers to stroke, that follow a pituitary tumor. It’s important to note that the benign tumor is often a warning that other disorders are soon to be on your doorstep and that you need treatment.
Most patients seek help and a diagnosis for many years, usually asking for medical help from family doctors, gynecologists, internists, neurologists, chiropractors, neurosurgeons and others. In far too many cases, medicine is prescribed, treatment is recommended or the patient is simply told, “There is an incidental finding of a micro-adenoma, but don’t worry, it is too small to be concerned about!” That is when you know that you are not in the office of an expert and you must find a new doctor.A large number of both prolactinomas and Cushing (ACTH) causing tumors, for instance, are too small to even be seen on an MRI. (30% or more don’t show up at all). An MRI is not the ideal way to diagnose a pituitary tumor. Your doctor should give you a physical exam, take a detailed medical history with a complete current condition, and use blood tests (sometimes urine also) or sputum (spit) to aid in diagnosis. An MRI (with a contrasting agent) is ideally used to determine the size and direction of growth of the tumor; a CAT scan just doesn’t have the same value or accuracy.
And yes, you can protect yourself. In addition, medical science is making rapid strides towards helping us. However, even good information travels slowly in the medical community, so your family doctor may not know about these advances for years after their discovery. It is up to you to stay informed. That is why the PNA was started.
Treatment
As with a complete and correct diagnosis, it is imperative that you be treated with the absolute competence of experienced endocrinologists, surgeons and radiologists, so you can be cured. That means, to get you back to the state of hormonal balance you enjoyed before the onset of your disorder. Sometimes this entails surgery, pharmaceuticals, radiation therapy or any combination of the three.
That being said; these experts can hopefully cure and/or control your disorders, but more than likely you’ll be a patient of some sort for the rest of your life. To get your blood/hormone readings into a normal range requires one set of skills; to repair your life and put your house in order is another skill set altogether, and one too often overlooked until very recently even by the very experts we admire. (They are now changing their opinions and recommendations, precisely because they are scientists, with an open and curious mind, welcoming new findings, opinions and knowledge.)
We also firmly believe that an appropriate treatment regimen must include the nurturing of the mind. It’s been understood throughout history, from Hippocrates to Dr. Harvey Cushing, that in the treatment of the body for various illnesses, one must not overlook the importance of caring for the mind. Earlier in this text, pituitary/hormonal disorders are likened to a slow-moving train wreck – and the damage can be every bit as dramatic and catastrophic. If you were to look carefully behind the door of each pituitary/hormonal diagnosis, you might find patients with shaky marriages, unstable friendships and family relationships, career lows, unfinished dreams, a collage of physical and psychosocial complaints, eating disorders, chemical dependencies, a history of depression and feelings of lingering worthlessness and apathy. It’s important to understand that beyond diagnosis and treatment, the patient must be solely responsible for the repair of these issues. This is done with therapy, pharmaceuticals, journaling, exercising and nutrition.
Reaching out to others in similar circumstances is helpful and recommended, as long as the environment remains positive. Letting go of lingering anger is an important part of moving life forward, as harboring negative feelings will breed anxiety and anger. Those feelings can not only lead to further illness, they poison everyone around you. This means different things to different people; for some it may be as simple as forgiving your doctor for not diagnosing and treating your disease early enough for your life to have a better quality. For others, it’s creating an understanding within your family that allows you to get well on your own time while keeping relationships intact. These are personal and individual issues and shouldn’t be dismissed.
The treatment, then, is far reaching and may touch on many seemingly unrelated issues in both body and soul. First and foremost; without accurate diagnosis your treatment may be worthless. Your endocrinologist will advise you on medication, surgery and radiosurgery as needed. At all times be aware that ONLY a highly trained and experienced physician and surgeon or radiologist is good enough. A referral to “the best doctor in town” may not be sufficient. You may have to go out of town or out of state or province in order to find the experts required. Careful treatment/examination could/should include a bone scan, dermatological evaluation, maybe a colonoscopy and most definitely an ophthalmologic exam, thorough, being the operative word!
Each case seems to be different. There are no quick fixes or cookie cutter approaches yet available for pituitary treatment.
Insurance Issues
It is logical that insurance carriers struggle against paying claims for two reasons, both of which are critical to understand in order to receive treatment, as well as for practical reasons, such as getting your doctors paid.
1) Insurance carriers earn money based on reserves required to pay claims on behalf of their policyholders. When the claims paid are less than the funds pooling in, that yields a profit. When claims paid are greater than funds pooling in, there will be a shortfall, which presents business issues for the insurance carrier, their financial holdings and stockholders. It’s commonplace for carriers to ‘hang on to claims’ for as long as possible, as the longer the funds are allowed to sit in reserves, the more money will be earned on the funds that are pooled. Many states have enacted legislative measures to ensure that claims are paid in a timely fashion (Medicare claims must be paid within a few weeks!) or the insurance company will be subject to fines and penalties. The rules differ from state to state but it’s not unusual for doctors in rural areas to reject insurance contracts unless they obtain favorable financial terms in writing, up front. What this means to you, as a pituitary patient, is that you will, without a doubt, have to fight to get your claims paid.
2) Few doctors truly understand pituitary/hormonal disorders and the same is true of insurance carriers. They must understand fully what they are paying for and your job is to inform them fully so they can help you. Much of the headache can be eradicated up front by taking a few simple steps: 1) have a copy of your insurance policy sent to you and read through the entire document, fine print and all. Knowledge is power, especially where insurance rights are concerned. 2) Obtain preauthorization in writing for any and all procedures up front, from both your insurance carrier as well as any third party administrator in charge of claims processing. 3) Ask your doctors for a list of codes he or she will be using and submit them to your carrier with an explanation as to what each means. 4) Keep a list of state and federal authorities who can jump in and help when you need them. (PNA members can access thiseasily through our website at www.pituitary.org)
Don’t forget to copy HR Directors when you write appeal letters. Their job is to handle insurance issues for their companies and group insurance policies renew on an annual basis. For policies of companies that are problematic, many companies will terminate contracts to get more favorable arrangements for employees. (The squeaky wheel gets the grease, so start squeaking!!)
You will often find that your insurance policy does not allow you to be treated by experts. Ignorance of the severity of the issues often stands between you and proper treatment. The failure of your insurance provider to understand medicine is not your fault. Therefore, it may be necessary for you to copy pages of information from this Resource Guide to help your insurance carrier understand what you are dealing with.
In each state in the US, and we hope in most provinces and countries there is an insurance commissioner or an appeals board that you can turn to for help. You may need an attorney to help you -not to file a lawsuit – but to negotiate on your behalf with the powers that be in order to ensure that you receive the best possible and most cost-effective treatment. Keep in mind that it is far less expensive to treat you correctly once, than haphazardly and incompletely treat you multiple times, often with dreadful results. Thousands of patients have been misdiagnosed (or under-diagnosed) and mistreated (or undertreated) multiple times, with financial, physical and emotional costs that are overwhelming to patients, to their families and friends, to employers and to society in general.
OUR ADVICE IS: FIGHT FOR YOURSELF. YOU MUST BE YOUR OWN ADVOCATE!
Rest of Life Care
With appropriate treatment and therapies, there is no reason why you should not live a long and happy life. In order to achieve this very commendable, yet achievable goal, it is imperative that you form a “rest of life” team of experts to keep an eye on you after the acute phase of treatment is over. The “thought leader” should be your endocrinologist. (You may only need to see him or her every year or two.) Your family physician should be kept in the loop regarding your treatments and he or she should coordinate notes and records with your endocrinologist as well as with the doctors who care for the other areas of your health, since any part of your body may affected by pituitary/hormonal disease (eyes, sexual health, emotional life, heart/lungs, skin, teeth, virtually everything). Check for cancer, regularly (breast, vaginal and prostate cancer in particular). Leave nothing to chance.
Emotional well-being
One aspect of pituitary/hormonal disease that is often overlooked, even by those with the very best of intentions, is mental/emotional health. It is a subject about which a few doctors know a lot, but most know very little. It is an issue of immense importance to you, your family, friends and society in general. It does not do anyone any good to “cure” you (chemically/hormonally) if you don’t also get well enough to function normally and rationally for the rest of your life! You are entitled to enjoy your life, job and family, and function as you did before. There is no shame in taking properly prescribed medicine which allows you to be calm, relaxed, sharp and functioning at normal speed. Paying attention to the well-being of your family relationships, career, and general social interaction is extremely important and must be a part of your recovery plan. Bridges which you may have thought were burned behind you forever can be rebuilt and relationships resumed.
Seek the help you need, from experienced professionals in all fields, and know that a pituitary/hormonal disease or tumor is NOT the end of the highway, merely a fork in the road. And, as Yogi Berra said: take it!
How Patients Can Help Prevent Misdiagnosis
By Tammy Mazzella, PNA
Recently a tweet caught my eye, and it reminded me about how important the right diagnosis really is. The tweet included a link to an article about misdiagnosis and how it is much more common than you think. Research shows that one in five people have some form of pituitary disease. We know that it sometimes takes years to get a proper diagnosis. The most interesting part of the story was that the problems start with lack of communication. Unfortunately, many people still consider pituitary and hormonal disorders to be rare. In most cases the patient has never heard of these disorders. In too many cases, neither have their doctors.
So, how can we get better care from our doctors? Well, if you are reading this, you have already made a good start. Joining the PNA is a great way to keep up with new breakthroughs in pituitary medicine. You will be connected to the medical experts available who have extensive experience in pituitary medicine. PNA membership also gives you access to a large community of people who understand what you are going through and can help guide you through your journey to better health. If you are not a member yet, join now! Work with us to help all pituitary patients get the attention of the medical profession and the health care industry.
Help us spread awareness about the symptoms and help other patients get an early diagnosis. You can refer to one of the most popular pages on the PNA website. It gives a list of symptoms:
-
-
- Headaches, particularly with a sudden onset and in the center of the head
- Sexual difficulties (painful intercourse, low libido, erectile dysfunction)
- Depression and/or changes in mood (anger, depression, anxiety), “bipolar” diagnosis
- Recent and or sudden onset of family, friend and/or relationship difficulties in conjunction with physical symptoms on this list including loss of relationships resulting in isolation, loneliness
- Infertility
- Growth abnormalities/changes especially of the hands (large fingers), feet, head, jaw and separation of teeth
- Obesity (especially in the central area of the body), especially weight gain over a short time, rounding or “moon face”, a large bump/hump on the back on the neck/back. Note: if you suddenly are unable to manage your weight with proper diet and increased activity/exercise, this is a hormonal red flag.
- Eating disorders: excessive weight loss, gain, bulimia. (Loss of interest in food or uncontrollable urges to eat.)
- Vision changes, including loss of peripheral vision, blurring etc., especially with sudden onset
- Skin thinning, stretch marks, bruising easily, acne and cuts or abrasions/pimples that don’t seem to heal
- Carpal tunnel syndrome
- Menstrual difficulties (irregular periods, discontinued, painful, no ovulation, anything not usual for your cycle), early menopause
- Fatigue, weakness in the limbs, general muscle weakness
- Hypertension
- Arthritis, aching joints, osteoporosis
- Loss of sleep, changes in sleep cycle
- Memory impairments, poor concentration
- Unusual hair growth (on chest, face etc.) or hair loss (falling out in clumps)
- Skin and hair that becomes extremely dry, scaly and discolored.
- Lactation not associated with pregnancy (breast leakage…even for men)
- History of emotional/physical trauma and/or chronic stress
- Depersonalization, i.e., feeling detached from one’s own body/mind
-
This is a huge list of symptoms and even if you have one or more of these symptoms, that doesn’t mean you have a pituitary tumor. However, you should immediately investigate further. Often, these symptoms are treated as individual problems and no one looks at the whole picture. Sometimes you need to step back a little for a better view. There is no one in the world who knows you like you do. Trust yourself, when you think something is wrong, take charge, and keep looking for answers until you find them. Don’t give up!
Make sure you communicate clearly with your doctors. Keep track of your symptoms, make a log, and be prepared for your appointments. Don’t just show up and expect the doctor to do all the work: do your part. Try to determine when your symptoms may have started; ask family and friends if they remember the onset of behavior changes or changes in your physical appearance. Look at old pictures of yourself for clues. Give your doctor as much information as you can. Help him or her treat you. Be involved in your health care. Be an active participant.
If you are not satisfied with your doctor’s answer, find another doctor! If you feel like you are getting the brush off, find another doctor! Keep looking until you find a doctor who will listen to you! I cannot emphasize enough the importance of finding the right doctor for YOU. You need to make sure that there is a good fit between you and your doctor. Remember that doctors work for you, so if you are not satisfied, say so. You wouldn’t hire a mechanic or contractor you don’t trust and believe in, so don’t stick with the wrong doctor, either.
Ask for what you think you need. Ask your doctor for the following medical tests (and request exact results, not just normal or abnormal).
-
-
- ACTH
- Cortisol
- Estradiol (E2) Extract/Testosterone
- GH
- FSH
- LH
- Prolactin
- Somatomedin-C (IGF-1)
- PSA (males)
- Free T3
- Free T4
- Total T4
- TSH
- 24 Hour urine FREE Cortisol (ideally 3 or more tests to rule-out error or hormone cycling).
-
If test results show problems or if the results are within “normal” ranges but you still have symptoms and are not getting answers you trust, then you must be seen by a physician that specializes in pituitary tumors and hormonal disturbances. These physicians are listed on the PNA website.
A mental health professional can also be a great asset. He or she can help you and your family deal with the strain of medical tests and with the struggle against the symptoms. Find a mental health professional that has some understanding of your physical state and a willingness to learn about neuroendocrine disorders. This is just as important as finding a medical professional with the same skills.
Finally, don’t be afraid to ask questions. Get the information you need. The Pituitary Network Association publishes the Pituitary Patient Resource Guide. If you don’t already have one, it is an invaluable tool in your quest for a better quality of life. Visit our website for more information about our Resource Guide and other tools available.
This is your life, your health. It is all about you! Take control!
Pituitary Disease and Disability
The PNA has received an article that gives tips for pituitary patients on applying for disability benefits from the Social Security Administration. This article was submitted by an advertising firm for attorneys who specialize in helping people apply for disability. While this information may be useful, the PNA would like to make it clear that the links they provide lead to their own website and are designed to attract clients. The Social Security Administration has a website that explains how to apply for disability directly. Click here to go the disability application page on the www.socialsecurity.gov site.
Here is the article:
Social Security Disability Benefits with Pituitary Disorders and Pituitary Tumors
If you have a pituitary disorder or pituitary tumor and you find you are unable to work because of the endocrine symptoms that your condition is causing, you can seek help through disability benefits. This will help you understand how you can apply for Social Security disability benefits and how the Social Security Administration (SSA) evaluates claims based on individual diagnosis.
Social Security Disability Programs
The SSA offers two disability benefits programs to disabled individuals, which are Social Security Disability Insurance (SSDI) and Supplemental Security Income (SSI). Each program has technical requirements that need to be met in addition to the medical criteria needed to qualify.
SSDI is funded by Social Security taxes and is meant for disabled workers who have paid in to the system from previous paychecks. You need to provide your work history and have earned enough work credits to qualify.
As of 2014, for every $1,200 earned you will receive one work credit, the maximum amount is four per year. For instance, you are required a minimum of 20 credits if you are 31 years or older to receive SSDI. The exact amount of work credits needed depends on your age.
SSI, on the other hand, is a need-based program for low-income individuals and takes into account the value of your total assets and resources. Instead of providing job history, you will need to prove that you meet the asset and income limits.
As of 2014, an individual cannot make more than $721 per month in income and cannot own more than $2,000 in assets, excluding the home and one vehicle.. The limitations increase for couples to $1,082 per month in income and $3,000 in assets. https://www.disability-benefits-help.org/content/social-security-programs
Medical Eligibility for Pituitary Disorders and Tumors
If you have a tumor or pituitary-related disorder, it may cause irregular hormone production. Either your pituitary gland will not produce enough of the necessary hormones or it may produce an excess of hormones. As a result, you may experience a range of medical complications. The symptoms depend on the severity of the problem, but typically you could suffer from one or more of the following symptoms:
• Loss of sleep, changes in sleep cycle
• Growth abnormalities
• Depression
• Headaches
• Memory loss, poor concentration
• Fatigue, weakness
• Hair loss
• Vision changes
• Irregular menstrual cycle
• Sexual dysfunction
Your treatment will depend on the disorder or type of tumor. Sometimes, removing the tumor can help to improve your condition. However, in some cases, people with a pituitary disorder or pituitary tumor don’t respond to treatment and end up with long-term disability that hinders their daily lives and livelihood. If you fall in this category, you could be eligible for Social Security disability to meet your treatment expenses and get a source of income. https://www.disability-benefits-help.org/disabling-conditions/pituitary-gland-disorders-and-social-security-disability
The SSA determines medical eligibility according to the Blue Book, which is a guidebook of all disabling conditions. Pituitary disorders and pituitary tumors are deemed disabling conditions under Section 9.00 – Endocrine Disorders. It states that if any individual suffers from hormone production disruption, which affects the normal functioning of the other endocrine glands then such an individual qualifies for benefits.
This said, it is important to remember the SSA evaluates each claim on a case-by-case basis and focuses on the severity of the symptoms. Therefore, if you need disability benefits, it’s important you get sufficient medical support to show the SSA your pituitary disorder or tumor is disabling.
Applying for Disability Benefits
You can apply for SSDI or SSI online or in person at your nearest Social Security office. During the application process, you will be asked to fill out a number of forms. It’s important to remember that you should provide as much evidence and support as possible to prove that your condition is indeed disabling.
Your answers should make it easy for the reviewer to understand how your pituitary disorder or tumor is affecting your day-to-day life and preventing you from earning an income. In addition, support the forms with copies of medical records, statements from the doctors, employment records, and financial information, among other things.
You should receive a letter around two to four months from the date of your application informing you of a decision. If you’re awarded benefits, you will be notified as to how much you will receive, when benefits will begin and what you’re entitled to. Also, two years after the SSA considers you disabled, you will qualify for medical benefits in the Medicare program.
On the other hand, if you’re denied, you have 60 days from the date of the notice to appeal the denial. It’s important not to stress, as many applicants get denied in the initial decision and go on to successfully receive benefits in the appeals process.
Legal Representation
If you need to appeal a denial of benefits, you may want to consider working with a disability attorney during the appeals process. Such professionals know the ins and outs of the application and appeal hearing process, and they will be able to represent your case effectively to help you get a favorable decision. Statistics show individuals who use disability attorneys have higher chances of a favorable outcome compared to those who don’t.
This application process can seem overwhelming, but the disability benefits can provide peace of mind and make more treatment options available to you.
Ask the Expert
The PNA recently asked for feedback on questions you’d like to have answered. Below are some questions from one of our readers, each followed by an answer from Dr. Manish Aghi, an eminent neurosurgeon at UCSF and a member of the PNA.
Question #1
I had a large pituitary adenoma – twice. It was apparently there for years, as symptoms date back to 15+ years before diagnosis. I’ve had two surgeries. When there is a large adenoma (mine was 3.5 cm) and it is very hard (mine was extremely fibrous, like a piece of raw ginger), and squashing of the hypothalamus and the bottom of the two brain lobes by the tumor over a period of many years, can that damage the hypothalamus? Does the hypothalamus “recover itself” over time, once the tumor is removed? Why don’t pituitary doctors etc. talk more about the whole HPA?
Answer #1
We have seen some examples of large adenomas causing compressive injury to the hypothalamus – there is some recovery capacity after surgery but these cases are rare enough that it is difficult to quote the chances of meaningful hypothalamic recovery after surgery.
Question #2
Why do many post-surgical patients still have some symptoms after tumor removal? For me, I have chronic pain, chronic inflammation, headaches, body temperature problems, and ongoing fatigue. I hear this from other pituitary patients all the time, but the medical establishment calls us “cured.” Seems to me there are long-lasting effects in some patients. Who is studying this? How is it quantified? Are there treatments to consider?
Answer #2
There are certainly some post-surgical patients who have symptoms after tumor removal and the patient is correct that we must not lose sight of these patients and merely consider them “cured.” If the symptoms were present preoperatively and don’t get better after surgery, they may be unrelated to the tumor, and this can be investigated by working with an endocrinologist or other specialist – we have certainly other problems in our pituitary patients such as fibromyalgia, polycystic ovarian disease, etc. An endocrinologist can also help determine if the patient’s gland function can be better optimized after surgery in case the symptoms are related to hypopituitarism that was either present preoperatively or is a new postoperative deficit. There are studies in which quantitative surveys looking at quality of life have documented some specific axes of deficiencies in some nonfunctional and functional adenoma patients before and after surgery, but these studies are descriptive and don’t necessarily give us any insight into the cause of these problems or how best to treat them.
Question #3
How does one go about “fine tuning” hormones after surgery? I was tested after surgery and every six months since, and my hormones are all within range – but just barely. Is micro-tuning an approach that should be considered, to bring my hormones into the middle of the zone? I am two years post-surgery now. My endocrinologist is in Los Angeles and I am in another state, and she (understandably) won’t treat me from afar. I can’t seem to find a qualified endo anywhere here, and my internist has tried looking too. Ideas?
Answer #3
There are times when being at the low end of normal but being symptomatic may require a trial of low dose hormone replacement but that is a decision best made working with an endocrinologist. Check the PNA’s site www.pituitary.org for listings in your state.
General Information for Pituitary Tumors
This article is reprinted from The Neurosurgical Atlas courtesy of Dr. Aaron Cohen-Gadol a physician member of the Pituitary Network Association. The original article and Dr. Cohen-Gadol’s webinar You Have Been Diagnosed with a Pituitary Tumor, What Next? can be accessed through this link.
What is a pituitary tumor/adenoma?
Pituitary tumors are most commonly benign tumors associated with one of the body’s most prominent hormone-secreting structures—the pituitary gland. The pituitary gland is located between your eyes and in the middle of the head at the base of skull. Pituitary tumors are slow-growing, non-cancerous, and will not spread to other parts of the central nervous system or body.
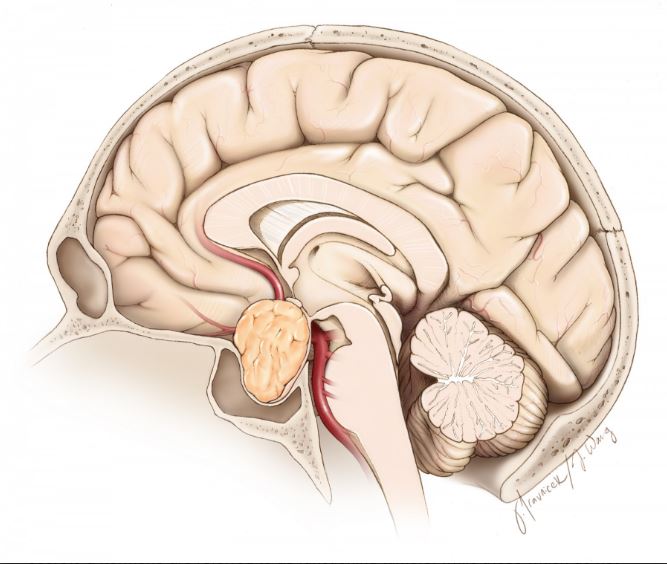
Cross section of a pituitary tumor
Pituitary tumors represent up to one-fourth of all brain tumors. These tumors may or may not secrete a variety of hormones on their own. The pituitary tumors which secrete a hormone are referred to as functioning tumors, while those which do not secrete a hormone are classified as nonfunctioning tumors.
Pituitary tumors are commonly referred to as pituitary adenomas.
What is a pituitary?
The pituitary gland plays an important role in hormonally regulating a wide-variety of body functions, such as growth, metabolism, sexual reproduction, water retention, and the body’s stress response. The stalk-like pituitary is surrounded by major arteries (the carotid arteries), the optic (eye) nerves, and important brain structures like the hypothalamus, which is responsible for regulating many of the body’s homeostatic (stabilizing) regulatory systems (including the pituitary).
Symptoms
The symptoms associated with pituitary tumors are generally a result of altered hormonal function and/or increased local pressure on the optic (eye) nerves caused by the tumor. Symptoms vary widely and depend on whether hormone secretion is altered, what kind of hormone is affected and overproduced, and which structures experience abnormal pressure and compression from the tumor.
Symptoms may be caused by pressure on the surrounding structures like the optic nerves or hypothalamus, or from decreased hormone output from the increased pressure on the pituitary gland itself.
Symptoms include:
- Headache
- Temperature sensitivity
- Excessive perspiration
- Decreased appetite
- Double vision, blurred vision, and/or poor peripheral vision
- Lethargy
- Nausea and vomiting
- Weakness
- Decreased libido
- Menstrual disorders
- Excessive thirst/frequent urination
- High or low blood pressure
- Constipation
- Slow-growth
- Late- or early-onset puberty
The remaining symptoms result from excessive levels of one of the following hormones.
Prolactin, which causes:
- Infertility
- Irregular or absent menstruation
- Decreased libido
- Production of milk and abnormal discharge from the nipples (galactorrhea)
- Osteoporosis
- Impotence
- Vaginal dryness
- Erectile dysfunction
Growth hormone, which causes:
- Enlargement of the hands, feet, face, tongue, and/or other soft tissues
- Gigantism
- Coarsening of facial features
- Sleep apnea
- Facial paralysis on one side
- Carpal tunnel syndrome
- Joint and bone pain
- Abnormal or excessive perspiration
- Oily skin
- Impotence
Adrenocorticotropic hormone (ACTH), which causes the symptoms of Cushing’s Disease:
- Rapid weight gain, particularly in the torso and face out of proportion to the limbs
- Insulin resistance leading to hyperglycemia and diabetes
- Thin and weakened skin that is prone to bruising
- Striae of the skin (lines/wrinkles/stretch marks)
- Hirsutism (facial and male-pattern hair growth)
- Psychological symptoms such as mood swings, depression, and anxiety
- Weakened muscles and bones
- Backache
- Hypertension
- Decreased fertility in men
Thyroid stimulating hormone, which causes:
- Increased appetite
- Weight loss
- Irregular heartbeat
- Tremors
- Fatigue
- Muscle weakness
- Insomnia
- Abnormally frequent bowel movements
- Swelling in the lower extremities
- Nervousness/irritability
- Decreased fertility
- Excessive sweating
Diagnosis
Pituitary tumors are found in men and women of all ages, although they are more common in older patients. The majority of tumors are not hereditary, although there are certain very rare hereditary conditions—such as multiple endocrine neoplasia, type 1 (MEN-1)—that increase the risk of developing such tumors.
Diagnosis is based on a variety of factors, including clinical history, physical examination and laboratory/radiological findings.
Your doctor will begin by taking a history in order to identify possible symptoms of pituitary disorders and eliminate alternative diagnoses. A physical examination is usually done to identify deficits in vision or changes in appearance that may be attributed to a pituitary tumor (Please see the changes associated with each hormonal imbalance above.)
Depending on what is found, the doctor may order a variety of tests:
Blood and/or urine tests are done to identify excessive or insufficient hormone levels.
An MRI (or less often, a CT) scan is performed to image the presence of a tumor. An MRI uses strong magnetic fields and radio waves to image soft tissues and detect a pituitary tumor.
Venous blood sampling may be used to detect ACTH-secreting tumors difficult to identify on MRI scans. This test is usually ordered when a patient presents with elevated ACTH levels but no tumor is found upon radiological examination. Blood is sampled from the venous drainage on both sides of the pituitary gland to test for abnormal ACTH levels; this can help identify an ACTH-secreting tumor, as well as which side it is located on.
Your doctor may also order a biopsy of the tumor if further identification is necessary; however, with pituitary tumors, other measures generally provide enough information to identify the tumor, and surgery or other treatment options are often pursued without a biopsy.
Treatments
Treatment options vary depending on the tumor type, size, and degree by which the tumor interferes with the surrounding structures. The three treatment options include:
- Medication
- Surgery
- Postoperative Care
- Radiation Therapy
- Medication
A variety of medications can be used to decrease the production of a specific hormone by the tumor or block the effect of that hormone on the body’s tissues. Additional medications may be used to substitute for low hormone production.
Prolactin-secreting tumors (called prolactinomas) usually shrink with medical therapy, negating the need for surgery.
Surgery
Surgery is the primary form of treatment for most pituitary tumors except for prolactin-secreting tumors. The type of surgery used and its chance of success depend on the tumor’s size, location and overall invasiveness.
Trans-sphenoidal adenomectomy is a surgical technique utilizing an endoscope to gain entry into the skull through the nose and remove your tumor, eliminating the need for an incision on the outside of the face. This is the preferred method for small, medium, and some of the even large sized tumors. There is no visible scar and no part of the brain is directly touched. This technique therefore minimizes neurological complications.
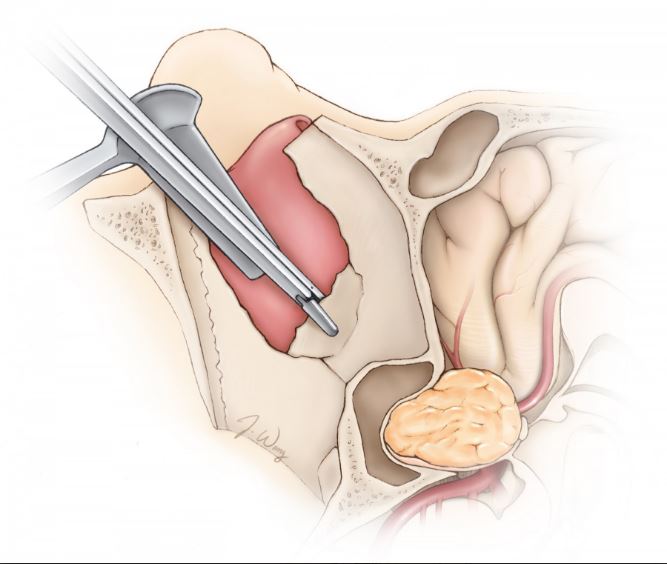
Endonasal approach to a pituitary tumor
Complication rates are low and most hospital stays are no longer than 1-2 days.
Some of the larger tumors usually cannot be removed in the same way. In such instances, the surgeon may opt for a transcranial adenomectomy. During this procedure, your surgeon exposes the tumor through the upper portion of the skull, through removal of a piece of the skull that will be replaced at the end of the surgery. This is a more invasive form of surgery and post-operative stays are longer—usually between three and four days.
Postoperative Care
The most common procedure is transsphenoidal surgery through the nose which approximately lasts about two hours (Please see video.) After surgery, there is remarkably little discomfort in and around your nose. There is packing in your nose that will be removed approximately 24 hours after surgery. You can usually be discharged from the hospital in 1-2 days after surgery.
During the surgery, the tumor is separated from the rest of the brain by a thin membrane (diaphragm.) If the tumor is large or if the tumor is adherent to this membrane, the membrane may slightly tear during tumor removal. This may cause leakage of brain fluid (cerebrospinal fluid, CSF) after surgery. If this is the case, your hospitalization will be prolonged as your surgeon will plan to repair the leak through placement of a small plastic tube (lumbar drain) in your back to divert the leakage and let the membrane (diaphragm) heal. A second short surgery may be rarely needed to fix the leakage.
During surgery, the back side portion of the pituitary gland may be irritated because of surgical manipulations during tumor removal. This portion of the gland may temporarily halt production of the hormone (ADH) which regulates your urine. Therefore, you may be urinating excessively for days after surgery and you will be given replacement hormone. This situation is usually temporarily and the use of hormone replacement for this purpose is brief.
Radiation Therapy
Radiation therapy is most commonly employed after you have had surgery to remove most of the tumor. It there is evidence of growth of the residual tumor after surgery, radiation treatment may be considered. Radiation therapy may come in the form of traditional external-beam radiation or via the more intense and precise stereotactic radiosurgery.
Traditional external-beam radiation therapy directly delivers a single beam of radiation to the tumor. The procedure is usually performed five times a week, for several weeks. The radiation treatments may take several years to bring tumor growth and/or hormone secretion under full control, and the procedure risks damaging normal pituitary function as well as adjacent neural structures.
Stereotactic radiosurgery can deliver higher doses of radiation more accurately by using precise computer imagery and multiple beams to target the tumor. It is does not require any incision and is done as a single-session outpatient procedure. As with external-beam radiation therapy, it may take years for the full benefits to manifest, but unlike external-beam radiation therapy, surrounding structures are less prone to damage from the radiation treatment (although the treatment is usually avoided for tumors near important nerves.)
Radiation therapy may be used rarely as an alternative to surgery in cases where the tumor is inaccessible via traditional routes. Tumor re-growth after surgery may also necessitate radiation treatment.
Prognosis
Most pituitary tumors are benign and slow growing (non-cancerous.) However, the tumors which produce certain hormones may have long-term side-effects that expose you to the risk of heart attack or stroke.
While usually not life-threatening, larger tumors can invade surrounding structures. The removal of these tumors is more challenging and they have higher tendency to recur.
Resources
National Cancer Institute Visit website
University of Pittsburgh Medical Center Visit website
Massachusetts General Hospital – Brain Tumor Center Visit website
National Institute of Neurological Disorders and Stroke Visit website
– See more at: https://www.neurosurgicalatlas.com/patient-resource-center/general-information-for-pituitary-tumors#sthash.legLuGre.dpuf
test
PNA Highlights July 2022
PNA Highlights July 2022

Happiness lies first of all in health.
George William Curtis
PNA Spotlight: Dr. Andre Beer Furlan
This month the PNA Spotlight focuses on Dr. Andre Beer Furlan, a skull base and endovascular neurosurgeon at Moffitt Cancer Center and Assistant Professor of Oncologic Sciences at the University of South Florida. Dr. Beer Furlan got his medical degree and a PhD from the University of São Paulo in Brazil. He stayed at the University of São Paulo to complete a neurosurgery residency. He practiced as a neurosurgeon and skull base surgeon in Sao Paulo and then moved to the United States, where he did a second neurosurgery residency at Rush University. He also did fellowships in skull base micro-neurosurgery at Weill Cornell Medical College, minimally invasive cranial surgery at Ohio State University and neuro-endovascular surgery at Rush University. He is fluent in English, Portuguese, Spanish and Italian. Dr. Beer Furlan was kind enough to answer a series of questions from the PNA; here are his answers.

Medical Corner: Adult Growth Hormone Deficiency
This month the PNA Medical Corner features an article co-authored by multiple members of the PNA, including Drs. Kevin Yuen, Lewis Blevins and Maria Fleseriu. The co-authors have developed an algorithm that combs a database and predicts which people would benefit from further testing to see if they have Adult Growth Hormone Deficiency.
• PMID: 35761982
• DOI: 10.1155/2022/7853786
Abstract
Objective: Adult growth hormone deficiency (AGHD) is an underdiagnosed disease associated with increased morbidity and mortality. Identifying people who may benefit from growth hormone (GH) therapy can be challenging, as many AGHD symptoms resemble those of aging. We developed an algorithm to potentially help providers stratify people by their likelihood of having AGHD.
Magnolia
PATHFNDR

Investigational Studies to Evaluate the Safety and Efficacy of Paltusotine in Patients with Acromegaly
The PATHFNDR studies are recruiting patients to participate in clinical research for once-daily paltusotine for the treatment of acromegaly. If the studies are successful, paltusotine could be approved as a ONCE-DAILY, ORAL treatment option that gives patients an alternative to injections or twice-daily oral medications.
As a study participant, you could play an important role in advancing the options available for acromegaly treatment for yourself and many others living with this rare disease.
ABOUT THE STUDIES
The purpose of the PATHFNDR studies is to see if Crinetics Pharmaceutical’s investigational medication, paltusotine, is safe and effective in patients with acromegaly.
PATHFNDR-1 is a randomized, placebo-controlled study designed to evaluate the safety and efficacy of paltusotine in
subjects with acromegaly treated with somatostatin receptor ligand (SRL) based treatment regimens. Clinicaltrials.gov
PATHFNDR-2 is a randomized, placebo-controlled study designed to evaluate the safety and efficacy of paltusotine in
subjects with non-pharmacologically treated acromegaly. Clinicaltrials.gov
1(855) 848-8486
Available Now!
The Pituitary Patient Resource Guide Sixth Edition is now available! Be one of the first to have the most up-to-date information. The Pituitary Patient Resource Guide a one of a kind publication intended as an invaluable source of information not only for patients but also their families, physicians, and all health care providers. It contains information on symptoms, proper testing, how to get a diagnosis, and the treatment options that are available. It also includes Pituitary Network Association's patient resource listings for expert medical care.

Xeris Pharmaceuticals is valued member of the PNA